- The need for cardiac pacing results from conduction disorders of the heart, which may or may not be associated with IHD.
- Permanent Pacemakers (PPM) are classified using a five letter code( See below)
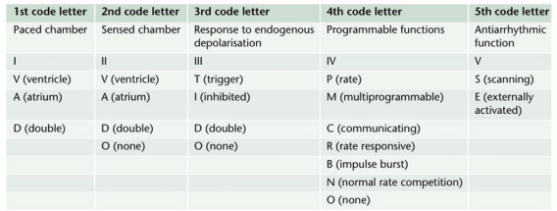
- For example DDDR means atrial and ventricular pacing (I), atrial and ventricular sensing(II) with double/adaptive (III) rate response(IV)
- Most modern units work in DDD mode, and provide atrial pacing in the presence of atrial bradycardia and ventricular pacing after an endogenous/paced atrial depolarization, if a spontaneous ventricular beat is absent
- KEY PERIOPERATIVE QUESTIONS: 1. Indication for pacemaker and associated cardiac comorbidities 2. Type of pacemaker; also how does the rate modulation work in that pacemaker? Chest x-ray will help to find the pulse generator siting and lead placement (atrium/ventricle/both) and number 3. When it was last checked 4. Requirement of diathermy for the procedure 5.Whether anticipating any other factor/s interfering with pacemaker function? 6. Surgical site proximity to the pacemaker 7. What is your plan to avoid inappropriate pacemaker function (e.g. change from demand to fixed rate mode) in case of interference? Cardiology/ Pacemaker programmer support may be needed for the same
- WHAT ECG CAN TELL: 1. If native rhythm predominates–> patient not PPM dependent 2. If all beats preceeded by a pacemaker spike–> pacemaker dependent 3. No evidence of pacemaker activity–> magnet might be applied over the pulse generator to switch to fixed rate pacing. If pacemaker is activated by a magnet to pace at a fixed rate, spike may fall in the refractory period and fail to stimulate the ventricle 4. If pacemaker spike is not followed by p or QRS waves –> PPM malfunction
- The characteristics of a PPM can be changed externally by application of a magnet or using radiofrequency generators, usually for a change of demand to fixed rate. Application of a magnet over a non-programmable VVI pacemaker will convert it to VVO asynchronous mode. The modern reprogrammable units need a cautious approach to the use of magnets. In this case, there is a risk of reprogramming ( with inappropriate settings), but it will remain in the asynchronous fixed rate mode, until the magnet is removed, after which the ‘inappropriate’ reprogrammed mode may take over
- ABOUT THE RATE RESPONSE FUNCTION: Such PPMs may sense electrical activity or vibration (e.g. shivering) and cause a tachycardia in response. Some measure respiratory rate by sensing thoracic impedence and adjust HR accordingly. Some sense blood temperature and so may cause a tachycardia when warming a hypothermic patient. With hypokalemia, there is a risk of loss of pacing capture and with hyperkalemia, there is risk of VT or VF.
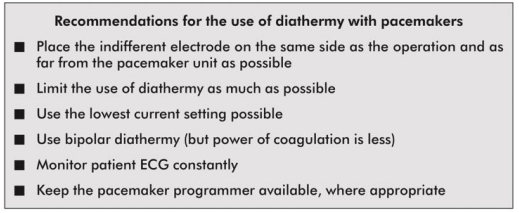
- INTRAOPERATIVE STEPS: 1. If possible, avoid surgical diathermy; but if unavoidable, bipolar is safer than unipolar diathermy. 2. Monopolar where necessary, should be used in short bursts with at as low energy levels as possible 3. Diathermy plate should be kept on the same side, as far away from the PPM as possible 4. Cables from diathermy equipment also should be kept away from the PPM 5. Confirm device functionality on completion of the surgery
- Surgical diathermy can cause 1. Ventricular fibrillation 2. ‘Reprogramming’ of programmable PPMs 3. Inhibition of demand function 4. Unit failure 5. Asystole
- AUTOMATIC IMPLANTABLE CARDIOVERTER DEFIBRILLATORS (AICDs) AND THE ANESTHESIOLOGIST: They consist of a set of lead electrode systems for sensing-pacing-delivery of shocks for cardioversion/ defibrillation; modern units can also function as DDD pacemakers. In general, AICDs better be deactivated with a programming device before surgery to avoid inappropriate shock delivery due to electrical interference; in modern AICDs, the anti-bradycardia function can be left activated (Consult the manufacturer for this). The effect of magnets are inconsistent across devices; but modern units are inhibited by magnets. If required, external pads can be placed over the patient with external defibrillators ready to attach, for use in case any tachyarrhythmias occur during this period. Take all precautions as in the case of PPM. Postoperatively, the ICD should be checked and reactivated.
Monthly Archives: June 2018
VIVA SCENE: DIATHERMY AND THE ANESTHESIOLOGIST
- WHY WE SHOULD KNOW? 1.Anesthesiologist may be blamed if burns occurs due to malposition of the plate 2. It can interfere with monitors e.g. ECG and pulseoximeters 3. It can disrupt pacemaker function in a patient, having it.
- Diathermy depends on the heat generated when a current pass through a tissue and is used to coagulate blood vessels and cut through tissues
- A high frequency current is necessary for this, as myocardium is sensitive to DC and low frequency AC [the usual mains frequency of 50 Hz] will precipitate VF. Very high frequencies have minimal tissue penetration and pass without harming the myocardium
- A 0.5 MHz alternating sinewave is used for cutting and a 1.0-1.5 MHz pulsed/ damped sinewave pattern is used for coagulation
- UNIPOLAR DIATHERMY & PROBLEMS: Here the forceps represent one electrode (small area, high current density and significant heat generation) and the diathermy plate ( indifferent electrode) over the patient represent the other electrode (large area, less heat). If the the plate is malpositioned, the current may pass through any point of metal contact *like ECG electrodes, metal poles of lithotomy, operation table etc, and may result in passage of high current density as the area of contact is small, resulting in a burn. So we should ensure that the plate is in close and proper contact with a large, highly perfused (will dissipate heat) area of skin (adhesive gels are useful). If we place it near to metal prosthesis (e.g. Hip), which has a low resistance than tissue, it will generate a high current density, resulting in burns. A unipolar diathermy can generate 150-400 Watts of energy.
- BIPOLAR DIATHERMY: Current passes between the two blades of the forceps; so requires no plate; safer in patients with pacemaker. But can generate only 40 Watts of energy. So efficacy is less and may be used for coagulation of small blood vessels
- OTHER PROBLEMS: Sometimes diathermies may cause ignition of skin preparation spirit. Newer diathermies dont have earthing; but if your machine is having earthing, an inappropriate earthing will result in current passing through other routes mentioned above*, resulting in burns.
- Cautious use of diathermy is required in patients with pacemakers:
VOCAL CORD PALSIES
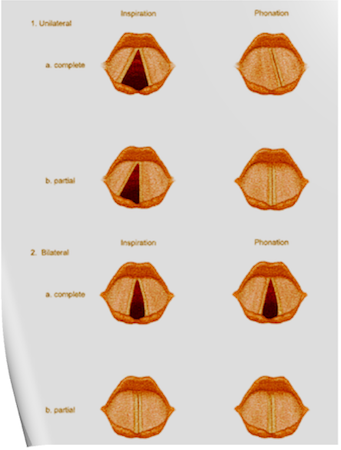
Under normal circumstances, the vocal cords meet in the midline during phonation. On inspiration, they move away from each other. They return toward the midline on expiration, leaving a small opening between them. When laryngeal spasm occurs, both true and false vocal cords lie tightly in the midline opposite each other.
The recurrent laryngeal nerve (RLN) carries both abductor and adductor fibers to the vocal cords.
Selmon’s law: The abductor fibers are more vulnerable, and moderate trauma causes a pure abductor paralysis. Severe trauma causes both abductor and adductor fibers to be affected. N.B.:- Pure adductor paralysis does not occur as a clinical entity.
Scenario 1- PURE UNILATERAL ABDUCTOR PALSY: As adduction is still possible on the affected side, the opposite cord come and meet in the midline on phonation. However, only the normal cord abducts during inspiration.
Scenario 2- COMPLETE UNILATERAL PALSY OF THE RLN: Both abductors and adductors are affected. On phonation, the unaffected cord crosses the midline to meet its paralyzed counterpart, appearing to lie in front of the affected cord. On inspiration, the unaffected cord moves to full abduction.
Scenario 3- BILATERAL INCOMPLETE ABDUCTOR PALSY: When there is incomplete bilateral damage to the recurrent laryngeal nerve, the adductor fibers draw the cords toward each other, and the glottic opening is reduced to a slit, resulting in severe respiratory distress.
Scenario 4- COMPLETE BILATERAL PALSY OF THE RLN: With a complete palsy, each vocal cord lies midway between abduction and adduction, and a reasonable glottic opening exists.
Thus, bilateral incomplete palsy is more dangerous than the complete variety.
Scenario 5- DAMAGE TO SUPERIOR LARYNGEAL NERVE/S: Damage to the external branch of the superior laryngeal nerve or to the superior laryngeal nerve trunk causes paralysis of the cricothyroid muscle (the tuning fork of the larynx), resulting in hoarseness that improves with time because of increased compensatory action of the opposite muscle. The glottic chink appears oblique during phonation. The aryepiglottic fold on the affected side appears shortened, and the one on the normal side is lengthened. The cords may appear wavy. The symptoms include frequent throat clearing and difficulty in raising the vocal pitch.
Scenario 6- TOTAL BILATERAL PARALYSIS OF VAGUS NERVES: This affects the recurrent laryngeal nerves and the superior laryngeal nerves. In this condition, the cords assume the abducted, cadaveric position. The vocal cords are relaxed and appear wavy. A similar picture may be seen after the use of muscle relaxants.
N.B:- Topical anesthesia of the larynx may affect the fibers of the external branch of the superior laryngeal nerve and paralyze the cricothyroid muscle, signified by a “gruff” voice. Similarly, a superior laryngeal nerve block may affect the cricothyroid muscle in the same manner as surgical trauma does.
Reference: Benumof and Hagberg’s Airway Management, Third edition
NITROUS OXIDE ISOTHERM
-
An isotherm is a line of constant temperature
-
Compressed gases in a cylinder can either stay as a gas, or change state to form a liquid due to the higher pressure (both carbon dioxide and nitrous oxide do this).
-
A graph of pressure against time for nitrous oxide is shown below. The isothermal lines are shown for 40°C, 36.6°C and 20°C.
-
At 40°C, nitrous oxide is above its critical temperature and so it is a gas no matter whatever pressure is being applied.
-
When it is compressed (moving from right to left along the isotherm) the pressure increases smoothly. At 36.6°C (the critical temperature), as soon as the pressure reaches the critical pressure (72 bar), the gas becomes a liquid.
-
At 20°C, once the pressure reaches 52 bar (the saturated vapour pressure of nitrous oxide at 20°C), some of the gas condenses so that liquid and vapour are both present. Further decreases in volume cause more vapour to condense, with no associated rise in pressure. When all the vapour has condensed to a liquid, any further reduction in volume causes a rapid rise in pressure.
-
In most circumstances, nitrous oxide is stored below its critical temperature of 36.4 C. It therefore exists in the cylinder as a vapour in equilibrium with the liquid below it.
-
To determine how much nitrous oxide remains in a given cylinder, it must be weighed, and the weight of the empty cylinder, known as the tare weight, subtracted. Using Avogadro’ s law, the number of moles of nitrous oxide may now be calculated. V/n= K, where V = volume of gas, n = amount of substance of the gas, K = a proportionality constant
-
Using the universal gas equation, the remaining volume can be calculated. PV = nRT, where P = pressure, V = volume, n = the number of moles of the gas, R = the universal gas constant (8.31 J/K/mol), T = temperature

CRITICAL TEMPERATURE AND PRESSURE
- Critical temperature: The temperature above which a gas cannot be liquefied regardless of the amount of pressure applied. (K/°C). At this point the specific latent heat is zero, as no further energy is required to complete the change in state of the substance.
- Critical pressure: The minimum pressure required to cause liquefaction of a gas at its critical temperature. (kPa/Bar)
- The latent heat of vaporisation is the heat energy required to change the state of a substance from liquid to vapour.
- At its critical temperature, a liquid will change spontaneously into vapour without heat being required. In other words, the latent heat of vapourisation is zero

GAS LAWS
- Boyle’s law
- At a constant temperature, the volume of a fixed amount of a perfect gas varies inversely with its pressure.
- PV = K or V ∝ 1/P . Also P 1 V 1 = P 2 V 2
- Ⓜ️NEMO> water Boyle’s at a constant temperature
- Example: P 1 V 1 relates to the pressure and volume in the cylinder and P 2 V 2 relates to the pressure and volume at atmospheric pressure. For example, oxygen is stored at 13 800 kPa (absolute pressure) in gas cylinders. If the internal volume of the cylinder is 10 litres, the volume this cylinder will provide at atmospheric pressure: 13 800 × 10 = 100 × V 2. So V 2 = 1380 litres. However, 10 litres will remain within the cylinder, so 1370 litres will be usable at atmospheric pressure.
- Charles’ law
- At a constant pressure, the volume of a fixed amount of a perfect gas varies in proportion to its absolute temperature.
- V/T = K or V ∝ T
- Ⓜ️NEMO> Prince Charles is under constant pressure to be king
- Gay–Lussac’s law (The third gas law)
- At a constant volume, the pressure of a fixed amount of a perfect gas varies in proportion to its absolute temperature.
- P/T = K or
- P∝T
- Perfect gas: A gas that completely obeys all three gas laws or A gas that contains molecules of infinitely small size, which, therefore, occupy no volume themselves, and which have no force of attraction between them.
- It is important to realize that this is a theoretical concept and no such gas actually exists. Hydrogen comes the closest to being a perfect gas as it has the lowest molecular weight. In practice, most commonly used anaesthetic gases obey the gas laws reasonably well.
- Other gas laws of relevance:
- Avogadro’s hypothesis: at a constant temperature and pressure, all gases of the same volume contain an equal number of molecules.
- Dalton’s law: the pressure exerted by a mixture of gases is the sum of the partial pressures of its constituents.
- Henry’s law: at a constant temperature, the amount of gas dissolved in a given volume of liquid is directly proportional to the partial pressure of that gas in equilibrium with the liquid.
- Henry’s law can be used to show that the amount of oxygen dissolved in blood is proportional to the partial pressure of oxygen in the alveolus. The amount of dissolved oxygen carried in blood is 0.023 ml·dl −1 ·kPa −1 . At atmospheric pressure, this accounts for a very small and insignificant fraction of oxygen delivery. However, under hyperbaric conditions, the dissolved fraction increases and becomes a more significant source of oxygen delivery to tissues
- At absolute zero, the theoretical volume of an ideal gas is zero. Real gases have liquefied before this point.
- Boyle’s, Charles’ and Gay-Lussac’s law are combined to form the ideal gas law.
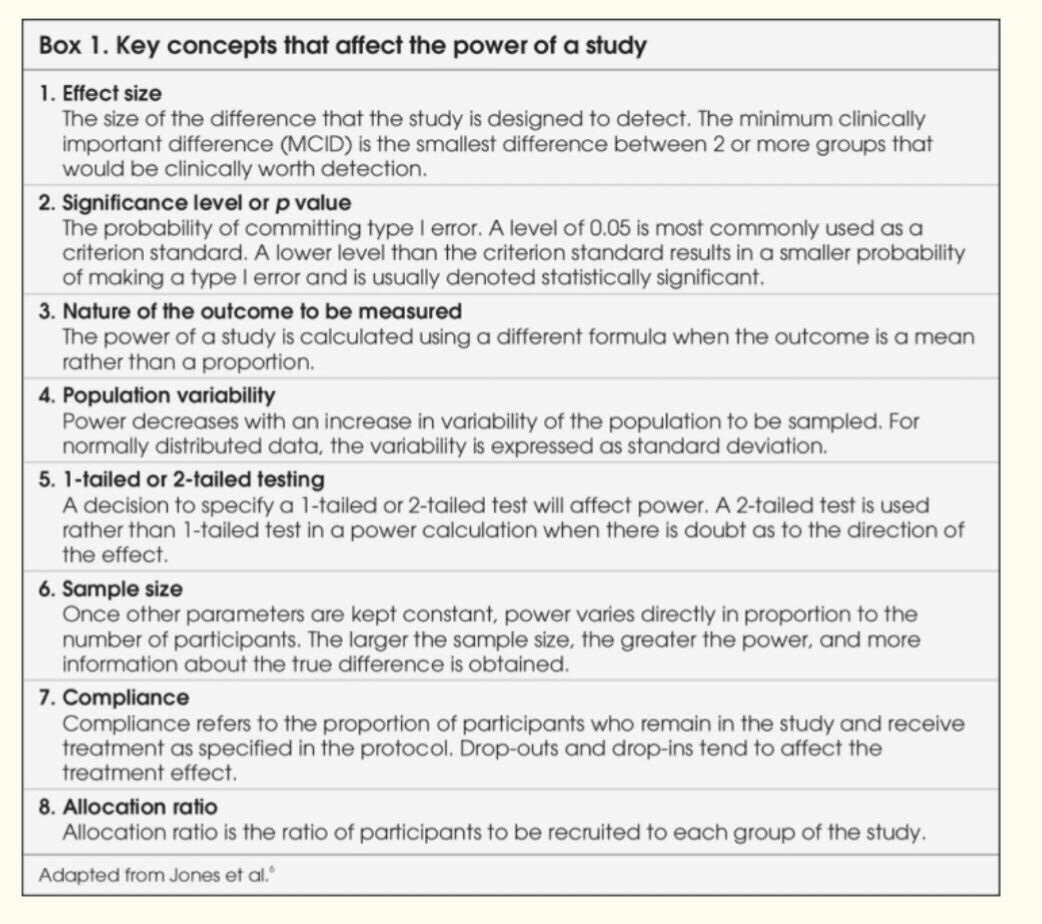
POWER OF A STUDY
🔸The power of a study is defined as “the ability of a study to detect an effect or association if one really exists in a wider population.”
🔸In clinical research, we conduct studies on a subset of the patient population because it is not possible to measure a characteristic in the entire population. Therefore, whenever a statistical inference is made from a sample, it is subject to some error.
🔸Investigators try to reduce systematic errors with an appropriate design so that only random errors remain. Possible random errors to be considered before making inferences about the population under study are type I and type II errors.
🔸To make a statistical inference, 2 hypotheses must be set: the null hypothesis (there is no difference) and alternate hypothesis (there is a difference).
🔸The probability of reaching a statistically significant result if in truth there is no difference or of rejecting the null hypothesis when it should have been accepted is denoted by type I error. It is similar to the false positive result of a clinical test.
🔸Type I errors are caused by uncontrolled confounding influences, and random variation. The probability of a type I error occurring can be pre-defined and is denoted as α or the significance level (represented by the p-value). The corresponding 1−α, or 95%, represents the specificity of the test.
🔸The p value may vary from 1 (the groups are the same) to 0 (100% certainty that the groups are different).
🔸In most clinical research, a conventional arbitrary value of P<0.05 is commonly used. This is an arbitrary figure which means that there is a 1 in 20 (5%) chance that there really is no difference between groups. Said in another way, if the null hypothesis is rejected, there should be a 5% chance of a type I error.
🔸As the p value becomes lower the possibility of there being ‘no difference when one has been found’ becomes more and more remote (e.g. p = 0.01, 1 in 100 and p = 0.001, 1 in 1000). Thus the lower the p value the less likely that a type 1 error has been made.
🔸As the sample size of a study increases, the P-value will decrease.
🔸The probability of not detecting a minimum clinically important difference if in truth there is a difference or of accepting the null hypothesis when it should have been rejected is denoted as β, or the probability of type II error. It is similar to the false negative result of a clinical test.
🔸The typical value of β is set at 0.2. The power of the study, its complement, is 1-β and is commonly reported as a percentage. Studies are often designed so that the chance of detecting a difference is 80% with a 20% (β = 0.2) chance of missing the Minimum Clinically Important Difference (MCID)
🔸This power value is arbitrary, and higher power is preferable to limit the chance of applying false negative (type II error) results.
🔸Type II errors are more likely to occur when sample sizes are too small, the true difference or effect is small and variability is large.
🔸The belief is that the consequences of a false positive (type I error) claim are more serious than those of a false negative (type II error) claim, so investigators make more stringent efforts to prevent this type of error
🔸At the stage of planning a research study, investigators calculate the minimum required sample size by fixing the chances of a type I or II error, strength of association and population variability. This is called “power analysis,” and the purpose is to establish what sample size is needed to assure a given level of power (minimum 80%) to detect a specified effect size.
🔸From this, one can see that for a study to have greater power (smaller β or fewer type II errors), a larger sample size is needed.
🔸Sample size, in turn, is dependent on the magnitude of effect, or effect size. If the effect size is small, larger numbers of participants are required for the differences to be detected.
🔸Determining the sample size, therefore, requires the MCID in effect size to be agreed upon by the investigators.
🔸It is important to remember that the point of powering a study is not to find a statistically significant difference between groups, but rather to find clinically important or relevant differences.
🔻N.B. The odds ratio is the ratio of the odds of the event happening in an exposed group versus a non-exposed group. The odds ratio is commonly used to report the strength of association between exposure and an event. The larger the odds ratio, the more likely the event is to be found with exposure. The smaller the odds ratio is than 1, the less likely the event is to be found with exposure.
Damping
- Damping describes the resistance of a system to oscillation resulting from a change in the input. Damping is the result of frictional forces working in that system. So following a change in input there are several possible outcomes for the system:
- Perfect Response: any change in input would be instantly and accurately reflected in the output
- Under-damped – the output changes quickly in response to the step up in input, but it overshoots and then oscillates around the true value, before coming to rest at it. It will take some time before the true value is displayed and the peaks and troughs will over and underrepresent the true value. In a dynamic system, e.g. intra-arterial BP, the constantly changing input may result in wild fluctuations, rendering an under-damped system very inaccurate (although the MAP is still correct).
- Critically damped – the response and rise time of the system are longer than an under-damped response, but there is no significant overshoot and oscillations are minimal. ‘D’ is the damping factor and, by convention, in a critically damped system D = 1.
- Over-damped – defined as damping greater than critical. The output here could potentially change so slowly that it never reaches the true value. In a dynamic system, the response time may be too slow for the system to be useful.
- Optimally damped – in reality in clinical measurement systems, critical damping is not ideal and we are prepared to accept a few oscillations and some overshoot to achieve a faster response time. Hence, our systems are ‘optimally damped’ where 64% of the energy is removed from the system and D = 0.64. There is a 7% overshoot in this case.
- N.B: The ‘response time’ is the time taken for the output to reach 90% of its final reading. The ‘rise time’ is the time taken for the output to rise from 10 to 90% of its final reading.
- All instruments will possess damping that affects their dynamic response. This includes mechanical, hydraulic, pneumatic and electrical devices. In an electromechanical device such as a galvanometer there are mechanical moving parts such as the meter needle and bearings. Damping in these components arises from frictional effects on their movement. This may arise unintentionally or may be applied as part of the instrument design to control oscillation of the needle when it records a measurement. In a fluid (gas or liquid) operated device, damping occurs due to viscous forces that oppose the motion of the fluid. In an electrical system, damping is provided electronically by electrical resistance that opposes the passage of electrical currents.
- Damping is an important factor in the design of any system. In a measurement system it can lead to inaccuracy of the readings or display:
- Under-damping can result in oscillation and overestimation of the measurement.
- Over-damping can result in underestimation of the measurement.
- Critical damping is usually an optimum compromise resulting in the fastest steady-state reading for a particular system, with no overshoot or oscillation.

Drowning: Specific points
- Drowning is death while submerged in water, and near-drowning is suffocation while submerged with survival (at least temporary).
- If water does not enter the airway, asphyxia is the main complication.
- If the patient inhales water, marked intrapulmonary shunting & significant V/Q mismatching because of loss of pulmonary surfactant (wash-out) and reflex laryngobronchospasm are also mechanisms
- Significant volumes of hypotonic fresh water aspiration can lead to hyponatremia and hemodilution.
- Cold water drowning leads to loss of consciousness at a temperature below 32°C and ventricular fibrillation can occur at 28° to 30°C. Resuscitation efforts may be very prolonged after cold water aspiration
- Aspiration of gastric contents because of unconsciousness and lack of airway reflexes can further complicate lung injury and risk of death.
- All patients will have hypoxemia, hypercarbia and metabolic acidosis from lack of oxygen delivery and subsequent lactic acid production.
- Also Cerebral edema, ALI, and ARDS can complicate medical courses
- Treatment: restore spontaneous circulation and ventilation, focus on improving oxygen delivery further to decrease metabolic acidosis. Because of a significant risk of ALI and ARDS, airway management and lung protection ventilation strategies should be initiated as soon as possible. Cerebral protection maneuvers should also be followed and neurosurgical consultation obtained when appropriate. Electrolyte and temperature derangements should be treated. Patients’ clinical courses will be labile.