- Its an ultra-short acting benzodiazepine that is currently under investigation in phase II and III clinical trials.
- It is metabolized by tissue esterases in the blood to its inactive metabolite, carboxylic acid, which allows for rapid removal of the drug even with its use in prolonged infusions.
- Remimazolam is eliminated by first-order pharmacokinetics, therefore with prolonged infusions or high doses, there is no problem with drug or metabolite accumulation .
- It has been evaluated as a premedication drug prior to anesthesia; however due to its very short duration of action and the fact that it is not available as an oral formulation limits its use in this clinical situation.
- It has been most studied as a drug for use in procedural sedation. It has been studied widely in sedation for endoscopic procedures like colonoscopies. Studies have shown doses of 0.1-0.2 mg/kg were effective sedative doses for patients undergoing endoscopic procedures. It allows for a faster onset and recover time when compared with midazolam. There is limited incidence of respiratory depression and it canability to be reversed with flumazenil without resedation
- It is also currently being studied as a general anesthetic, using induction doses of 6 and 12 mg/kg/h and maintenance rates of 1 mg/kg/h.
- Because its metabolism is organ-independent, it also has been evaluated for use as a sedative agent in the ICU setting. Its ultra-short acting nature would also make it an ideal agent to allow for neurological evaluation very soon after an infusion has been stopped .
- The safety profile of remimazolam has been shown to be favorable overall, demonstrating less vasopressor use compared with patients sedated with propofol
Monthly Archives: October 2018
ETOMIDATE- BAD ‘WOW’ FACTORS
- While it continues to be used infrequently in the UK it has been withdrawn in North America and Australia
- The most notable and potentially serious side effect of etomidate administration is the suppression of adrenocortical steroid synthesis.
-
It suppresses adrenocortical function by inhibition of the enzymes 11-hydroxylase and 17-hydroxylase, resulting in inhibition of cortisol and aldosterone synthesis.
- After a single bolus dose of etomidate, this adrenocortical suppression lasts approximately 6 h in healthy individuals. However in the critically ill, such suppression can last for days. In other words the situation in which it has the best cardiovascular proile is the unwell patient in whom the consequences of steroid inhibition are likely to be the most detrimental.
- Etomidate is approximately 100-fold more potent a suppressor of adrenocortical function than it is a sedative-hypnotic. Consequently, an anesthetic
-
induction dose of etomidate represents a massive overdose with respect to its ability to suppress adrenocortical function. And etomidate’ s terminal elimination half-life is rather long. Thus, after just a single anesthetic induction dose of etomidate, many hours must pass before etomidate’ s concentration in the blood falls below that which suppresses adrenocortical steroid synthesis.
-
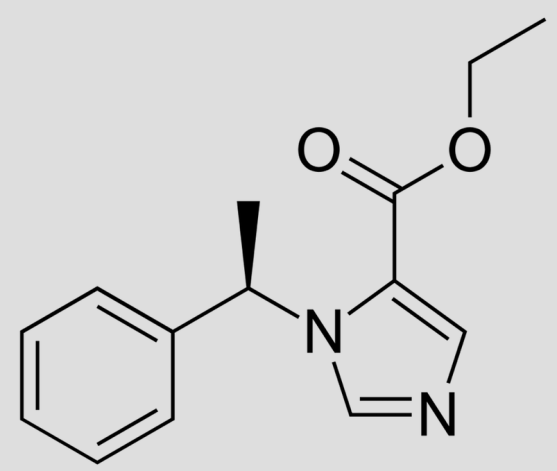
It is within this mechanistic context that the strategy emerged to design analogues of etomidate
- ANALOGUES:
- MOC-etomidate [ relatively low potency and very rapid metabolism (1.) required the administration of extremely large doses]
- CPMM etomidate [ it has an onset and offset of hypnotic action that are fast (1.) ]
- Carbo etomidate [ less adrenocortical inhibition (2.)]
- MOC-carboetomidate [ combines properties (1) and (2); but it’s potency
-
is very low which means that extremely large doses would need to be administered to maintain anesthesia ]
-
Involuntary movements (myoclonus) are commonly observed after etomidate administration, with some studies reporting an incidence as high as 80 % in unpremedicated patients
- It has been suggested that it occurs because etomidate depresses inhibitory neural circuits in the central nervous system sooner and at lower concentrations than excitatory circuits.
-
Regardless of the mechanism, myoclonus can be significantly reduced or completely prevented by administering a variety of drugs with central nervous system depressant effects including opiates, benzodiazepines, dexmedetomidine, thiopental, lidocaine, and magnesium.
-
Pain at the injection site is another common side effect and its incidence is highly dependent upon the size of the vein into which it is injected and the formulation that is used.
-
Lipid emulsion and cyclodextrin formulations may reduce TRP channel activation, leading to less pain on injection
-
Postoperative nausea and vomiting is common with reported incidences as high as 40 %. It has been suggested that the emetogenic trigger in etomidate is the propylene glycol solvent and not the anesthetic itself.
-
Reference: Ref: Pharmacology for Anaesthesia and Intensive Care, Peck and Hill, 4/e, p:105, Total Intravenous Anesthesia and Target Controlled Infusions, A comprehensive global anthology, Anthony R Absalom