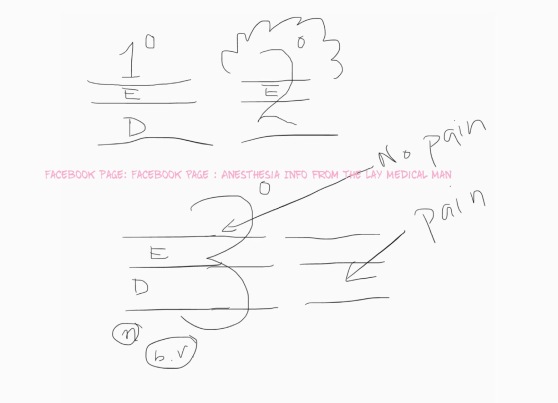
- First degree burns don’t penetrate the epidermis and the areas of involvement should not be considered when calculating for fluid volume for resuscitation
- Second degree burns penetrates the epidermis & extends into the dermis and will cause blisters
- Third degree burns involve epidermis, full thickness of dermis, deeper tissues, blood vessels and nerves
- The “rule of nines” is used to calculate the total body surface area (TBSA) .
- The Parkland formula recommends 4 mL/kg/% TBSA burned, to be given in the first 24 hours (half of this should be given in the first 8 hours and the rest over the following 16 hours).
- The Modified Brooke protocol recommends 2 mL/kg/%TBSA.
- Fluid leak may occur when patients are given volume beyond the intended calculations. This can lead to abdominal compartment syndrome, pulmonary edema, or pneumonia.
- Carbon monoxide (CO) poisoning should be considered in all major burn injuries.
- CO binds to hemoglobin (HbCO) with an affinity of 250 times that of oxygen and shifts the oxygen–hemoglobin dissociation curve to the left.
- Pulse oximetry causes falsely elevated oxygen saturation because it is unable to distinguish HbO from HbCO, as CO-Hb has similar absorption spectra as that of oxy-Hb
- HbCO levels below 10% are not usually clinically significant, levels of 20% may require mechanical ventilation, and death from CO poisoning occurs at HbCO levels of 60%.
- In cases where CO poisoning is suspected, treatment should be with highflow 100% oxygen, which increases the speed of elimination of CO. Hyperbaric chambers are used to further increase the speed of CO removal.
- Burns patients have an inability to regulate body temperature and must be kept warm.
- Urgent airway management may be indicated by the presence of a hoarse voice, dyspnea, tachypnea, or altered level of consciousness.
- Succinylcholine can cause lethal elevations in potassium after the first 48 hours.
Monthly Archives: June 2017
SYMPATHETIC GANGLIA & CHAIN
PREGANGLIONIC NEURONS of the sympathetic system synapse with the POSTGANGLIONIC NEURONS in the SYMPATHETIC GANGLIA. These ganglia together will form sympathetic chain. The sympathetic chains extend down the length of the vertebral column and are divided into four parts:
CERVICAL SYMPATHETIC GANGLIA
🔸Consist of three ganglia: Superior, Middle and Inferior
🔸Superior sends postganglionic fibres to form the internal carotid plexus
🔸Inferior or Stellate ganglion is fused with the first thoracic ganglia
THORACIC SYMPATHETIC GANGLIA
🔸T1-T5 ganglia supply the aortic, cardiac and pulmonary plexus
🔸The last 7 thoracic ganglia form the greater and lesser splanchnic nerves
🔸The lowest splanchnic nerve is formed from the last thoracic ganglia and supplies the renal plexus
LUMBAR PREVERTEBRAL SYMPATHETIC GANGLIA
🔸Supplies the coeliac plexus
SACRAL SYMPATHETIC GANGLIA (PELVIC)
🔸Contribute to hypogastric and pelvic plexus
THE AUTONOMIC NERVOUS SYSTEM (ANS) IN GENERAL: RANDOM POINTS RELEVANT FOR THE ANESTHESIOLOGIST
➿The autonomic nervous system is a division of the nervous system that controls the activity of internal organs.
➿The sympathetic division prepares the body for fight or flight reactions. The parasympathetic system promotes ‘rest and digest’ (restorative) functions.
➿Acetylcholine is the principal transmitter released by the preganglionic fibres of both the sympathetic and the parasympathetic nervous systems. The parasympathetic postganglionic fibres secrete acetylcholine onto their target organs, whereas norepinephrine is principally secreted by the postganglionic sympathetic fibres.
➿The central portions of the autonomic nervous system are located in the hypothalamus, brainstem and spinal cord. The limbic system and parts of the cerebral cortex send signals to the hypothalamus and lower brain centres, which can also influence the activity of the ANS
➿The posterior and lateral hypothalamic areas increase blood pressure and heart rate, whereas the preoptic area decreases blood pressure and heart rate. These effects are mediated by cardiovascular centres in the pontine and medullary reticular formation.
➿In the ANS, the connection between the CNS and its effector consists of two neurons—the preganglionic neuron and the postganglionic neuron. The synapse between these two neurons lies outside the CNS, in an autonomic ganglion [These are the cell bodies of the post ganglionic neuron, located in chains alongside the vertebral column, in plexuses in the abdomen (Sympathetic) or within the innervated target organ (Parasympathetic)]. The axon of a preganglionic neuron enters the ganglion and forms a synapse with the dendrites of the postganglionic neuron. The axon of the postganglionic neuron emerges from the ganglion and travels to the target organ #TheLayMedicalMan
➿The sympathetic system has short preganglionic fibres and long postganglionic fibres. As the parasympathetic ganglia are located near or within their effector organs, the parasympathetic postganglionic fibres are short.
➿ The pre-ganglionic fibres are slow-conducting B or C fibres. The postganglionic fibres that originate from the ganglia and innervate target organs are largely slow-conducting, unmyelinated C fibres. #TheLayMedicalMan
➿ There are more postganglionic fibres than preganglionic nerves and so the stimulation of a single preganglionic neuron can activate many postganglionic nerves, resulting in divergence. But in the superior cervical ganglion, numerous preganglionic fibres converge on a single postganglionic neuron, resulting in convergence.
Facebook page : Anesthesia Info from The Lay Medical Man
THE PARASYMPATHETIC NERVOUS SYSTEM: POINTS RELEVANT FOR THE ANESTHESIOLOGIST
🎳The anterior hypothalamus controls the parasympathetic nervous system
🎳The posterior and lateral hypothalamic areas increase blood pressure and heart rate, whereas the preoptic area decreases blood pressure and heart rate.
🎳The parasympathetic nervous system arises from neurons in the brainstem and spinal cord sacral segments (S 2 –S 4 ). As the parasympathetic ganglia are located near or within their effector organs, the parasympathetic postganglionic fibres are short, and they all release acetylcholine. The distribution of parasympathetic outflow is restricted so that parasympathetic effects are more localized than sympathetic effects.
🎳Cranial nerves 3, 7, 9 and 10 have parasympathetic components (3 – pupil and ciliary body constriction; 7 – tearing and salivation; 9 -salivation: 10 – the vagus and its ramifications).. Preganglionic fibres of the third cranial nerve arise from the oculomotor nucleus and pass through the orbit to the ciliary ganglion. Postganglionic fibres from the ciliary ganglion supply the ciliary muscle and sphincter of the iris and constrict the pupils.
🎳Preganglionic fibres from the superior salivary nucleus of the seventh nerve form the chorda tympani and reach the submaxillary ganglion via the lingual nerve. Postganglionic fibres supply the submaxillary and sublingual salivary glands and cause salivary secretion. #TheLayMedicalMan
🎳Preganglionic fibres arising from the inferior salivary nucleus of the ninth nerve form the lesser superficial petrosal nerve and reach the otic ganglion. The postganglionic fibres are distributed to the parotid gland via the auriculotemporal nerve and also cause salivary secretion.
🎳The vagus nerve is the major part of the cranial parasympathetic outflow. The preganglionic fibres arise from the dorsal nucleus of the vagus in the medulla and terminate in the ganglia of plexuses or in the walls of visceral organs. Postganglionic fibres supply the heart and decrease cardiac excitability, contractility, conductivity and rate. Postganglionic fibres from the pulmonary plexus contract the circular muscles of the bronchi, producing bronchoconstriction. Vagal branches to the gastric plexus give rise to postganglionic fibres to the stomach, liver, pancreas and spleen. Stimulation of the vagus causes increased gastric motility and secretions, with relaxation of the pyloric sphincter. The intestinal branches of the vagus supply the small and large intestines down to the transverse colon and it’s stimulation increases peristalsis and relaxes the ileocolic sphincter. #TheLayMedicalMan
🎳 The sacral outflow of the parasympathetic system arises from the second, third and fourth sacral segments of the spinal cord, and fibres enter the hypogastric plexus to innervate the descending colon, rectum, bladder and uterus. It’s stimulation contracts the muscular wall of the rectum, relaxes the internal sphincter of the anus and contracts the detrusor muscle of the bladder wall.
Ref: Principles of Physiology for the Anaesthetist , 3/e
#physiology , #anaesthesia
THE SYMPATHETIC NERVOUS SYSTEM: POINTS RELEVANT FOR THE ANESTHESIOLOGIST
🔸Posterior hypothalamus is the principal site of sympathetic nervous outflow.
🔸The sympathetic system has short preganglionic fibres and long postganglionic fibres
🔸The sympathetic nerves originate from columns of preganglionic neurons in the grey matter of the lateral horn of the spinal cord from the first thoracic segment down to the second or third lumbar segment.
🔸’BASIC CIRCUIT’ : PREGANGLIONIC NEURONS in the grey matter of the lateral horn of the spinal cord (from T1-L3 segment) –> they leave the spinal cord through the VENTRAL roots with the spinal nerves and then leave the spinal nerves as WHITE RAMI COMMUNICANTES (myelinated B fibres)–> they then synapse with the POSTGANGLIONIC NEURONS in the GANGLIA OF THE SYMPATHETIC CHAIN –> These ganglia together will form sympathetic chains –> The POSTGANGLIONIC NEURONS leave the ganglia as GREY RAMI COMMUNICANTES (unmyelinated C fibres) and join the spinal nerves or visceral nerves to innervate the target organ.
🔸In general, the preganglionic fibres secrete acetyl choline as neurotransmitter, while the post ganglionic ones secrete norepinephrine. The postganglionic sympathetic nerves that innervate the blood vessels of muscles, sweat glands and the hair follicles in the skin release acetylcholine instead of norepinephrine (noradrenaline).
➡️ The sympathetic chains extend down the length of the vertebral column and are divided into four parts:
🔸A cervical part consisting of superior, middle and inferior galglia, supplying the head, neck and thorax. The superior cervical ganglion sends postganglionic fibres to form the internal carotid plexus. The inferior cervical or stellate ganglion is fused with the first thoracic ganglion.
🔸Branches of the thoracic part, from T1 – T5 supply the aortic, cardiac and pulmonary plexuses. The greater and lesser splanchnic nerves are formed from the lower seven thoracic ganglia. The lowest splanchnic nerve arises from the last thoracic ganglion and supplies the renal plexus.
🔸The coeliac plexus is derived from the lumbar sympathetic ganglia
🔸The sacral ganglia contribute to the hypogastric and pelvic plexus #TheLayMedicalMan
SYMPATHETIC SYSTEM UNIQUE EFFECTS:
DILATATION / RELAXATION
✔️Pupils
✔️Bronchial smooth muscle
✔️Gut, Urinary bladder (sphinctors constrict)
✔️Skeletal muscle arterioles (Post ganglionic transmitter: ACh)
CONSTRICTION / SECRETION
✔️Levator Plapabrae Superioris
✔️Piloerection hair follicle (Post ganglionic transmitter: ACh)
✔️Muscles of seminal vesicles(ejaculation)
✔️Sweat glands (sweating) (Post ganglionic transmitter: ACh)
#physiology , #anaesthesia
