Category Archives: Drugs and Pharmacology
SAFE & APPROPRIATE ADMINISTRATION OF TIVA
Anaesthesia Exam Podcast: Crystalloids vs Colloids
Bridging Anticoagulation
Bridging anticoagulation consists of the substitution of a long-acting anticoagulant (usually with warfarin) for a shorter-acting anticoagulant (usually LMWH) to limit the time of subtherapeutic anticoagulation levels and minimize thromboembolic risk. Despite the growing evidence about the limited to nonexistent benefits of bridging therapy, it is still being used on a case-by-case basis. Clinical scenarios that may benefit from bridging therapy are those involving patients with high thromboembolic risk. In several guidelines, the following scenarios have been proposed:
- The patient with a mechanical heart valve: Mitral valve replacement, aortic valve replacement with additional risk factors (stroke, TIA, cardioembolic event, or intracardiac thrombus), more than 2 mechanical valves.
- Patients with stroke, episode of systemic emboli, or VTE during the last 3 months. Patients presenting with a thromboembolic event after interruption of chronic anticoagulation therapy or those presenting with VTE while on therapeutic anticoagulation.
- Patients with atrial fibrillation and CHA2DS2VASc score > 5 plus additional cardiovascular risk factors (rheumatic valve disease, stroke, or systemic embolism within the last 12 weeks). A CHA2DS2VASc score > 6 with or without additional risk factors.
- Patients with recent coronary stenting (within the previous 12 weeks)
How to bridge?
During the preoperative period:
- Discontinue warfarin five days before surgery.
- Three days before surgery, start subcutaneous LMWH or unfractionated heparin (UFH), depending on the renal function of the patient at therapeutic doses.
- Two days before surgery assess INR, if greater than 1.5 vitamin K can be administered at a dose of 1 to 2 mg.
- Discontinue LMWH 24 hours before surgery or 4 to 6 hours before surgery if UFH.
During the postoperative period:
- If the patient is tolerating oral intake, and there are no unexpected surgical issues that would increase bleeding risk, restart warfarin 12 to 24 hours after surgery.
- If the patient received preoperative bridging therapy (high thromboembolic risk) and underwent a minor surgical procedure, resume LMWH or UFH 24 hours after surgery. If the patient underwent a major surgical procedure, resume LMWH or UFH 48 to 72 hours after surgery.
- Always assess the bleeding risk and adequacy of homeostasis before the resumption of LMWH or UFH
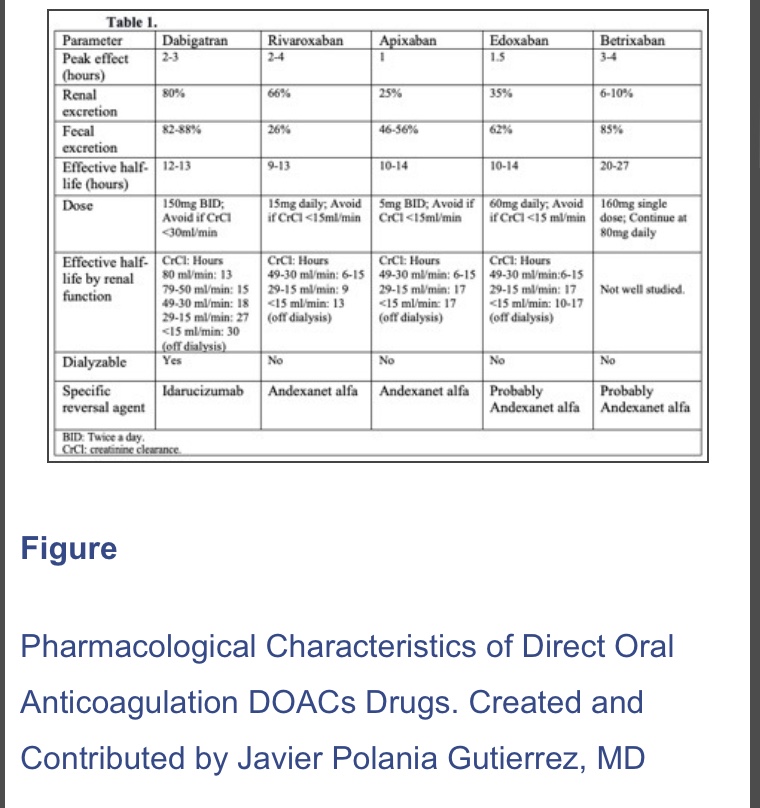
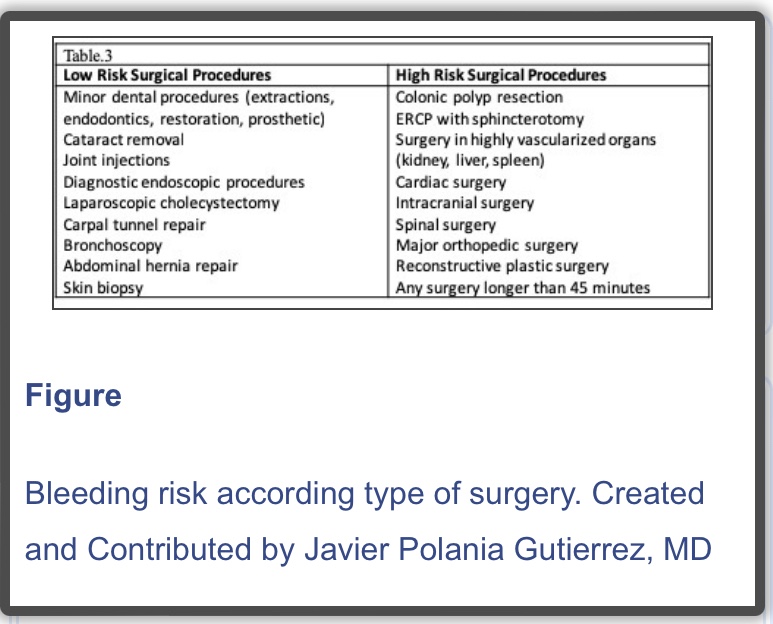
N.B. : In 2019, a new strategy was published in the PAUSE study, a prospective clinical trial evaluating a standardized approach for perioperative management of DOACs. The interruption scheme used in this study was simple. For high bleeding risk procedures, rivaroxaban, apixaban, and dabigatran were suspended 48 hours before surgery in patients with CrCl>50 ml/min. If the renal function was compromised (CrCl< 50 ml/min), these drugs were interrupted for four days before surgery. For low bleeding risk procedures, rivaroxaban, apixaban, and dabigatran were interrupted 24 hours before surgery in patients with CrCl>50 ml/min. If the renal function was compromised (CrCl <50 ml/min), drugs were suspended two days before the procedure. Regardless of renal function, all drugs were reinitiated at 48 hours for high bleeding risk surgical procedures and 24 hours for low bleeding risk procedures. The 30-day postoperative rate of major bleeding was 1.35% (95% CI, 0%-2.00%) and rate of arterial thromboembolism of 0.16% (95% CI, 0%-0.48%). However, more studies are needed in patients with high surgical bleeding risk, before implementing this in regular clinical practice
Reference:
Perioperative Anticoagulation Management – StatPearls – NCBI by Polania Gutierrez JJ, Rocuts KR. · 2021
https://www.ncbi.nlm.nih.gov/books/NBK557590/
Volume of Distribution
- Is the theoretical volume into which a drug must distributes to produce the measured plasma concentration
- Unit is mL
- It is measured as Vd= Dose / Co, where Co is the initial plasma concentration from a concentration-time graph
- Lipid solubility, plasma protein binding, tissue protein binding, regional blood flow etc determine the Vd
Acidic and Basic drugs
DO YOU KNOW❓
3 drugs with delayed recovery are weak bases: Diazepam, Midazolam & Etomidate (pKa ranging from 3-6)
5 drugs which are potent analgesics are strong bases: Morphine, Fentanyl, Ketamine, Bupivacaine, Lignocaine (7.5-8.5)
4 most commonly used drugs are weak acids: Paracetamol, Propofol, Atropine, Thiopentone (7.5-11)
LASI (lasix) and SALI (salicylic acid) are strong acids (3-4)
At pH < pKa, acidic drugs become less ionised:
HA ⇌ H+ + A–
At pH < pKa, basic drugs become more ionised as they accept protons:
B + H+ ⇌ BH+
Drugs cross membranes in the un-ionised state and so their pKa and the pH of the surrounding environment affect their rate of absorption. Hence, acidic drugs will be more readily absorbed in the highly acidic stomach, whereas basic drugs are better absorbed in the intestine where pH is higher.
Note: You can not find from pKa whether a drug is acidic or basic
Antiepileptic of Choice
FOCAL SEIZURE: Lamotrigine, Carbamazepine, Oxcarbamazepine
GENERALISED TONIC CLONIC SEIZURE (GTCS): Sodium Valproate/Lamotrigine/levetiracetam/zonisamide/topiramate
ABSENCE SEIZURE: Ethosuximide/ Sodium Valproate, Lamotrigine (Carbamazepine may exacerbate)
MYOCLONIC SEIZURE: Sodium valproate/ Levetiracetam/ Topiramate/ Zonisamide (Carbamazepine, Lamotrigine may exacerbate)
TONIC/ATONIC SEIZURE: Sodium valproate/Lamotrigine/Phenytoin
INFANTILE SPASMS: Steroids (Prednisolone)/ Vigabatrin
Lennox–Gastaut syndrome: Sodium Valproate/Lamotrigine
(Do not offer sodium valproate to women and girls of childbearing potential)
[Ref: NICE guidelines 2012; last update: 2021 ]
PHENTOLAMINE
- Competitive alpha blocker
- Used in hypertensive emergencies like in pheochromocytoma; also in CRPS
- MOA: 3 times more specific for alpha 1 receptors than alpha 2. Doesn’t bind covalently to receptors; hence reversible. Also has beta agonistic and anti-serotoninergic activity
- Comes as pale yellow solution 10 mg/mL; dose is 1–5 mg titrated to effect
- CVS: Vasodilation and reduce BP, improve coronary artery perfusion, reduce pulmonary artery pressures. Alpha 2 blockade enhances noradrenaline release causing increase in HR and CO
- RESPIRATORY SYSTEM: Increase FEV1, increase secretions, prevents bronchospasm caused by histamine release
- Other Side Effects: Nasal congestion, Hypoglycemia (Causes insulin secretion)
PHENOXYBENZAMINE
- Phenoxybenzamine is a haloalkylamine. Used as a vasodilator in hypertensive emergencies like in pheochromacytoma; also used in the management of CRPS. Used in the management of intraarterial injection of thiopentone too.
- It is a non-selective alpha blocker. It binds covalently to the receptors. So it behaves like a competitive irreversible antagonist.New receptors must be synthesised to overcome drug effect. Blockade of alpha 2 receptors increases the amount of noradrenaline released: produces tachycardia. Partial agonist at 5-HT2 receptors
- Available as capsules of 10 mg and solution: 50 mg/mL for iv use. Oral dose is 10–60 mg per day in divided doses and IV: 10–40 mg over 1 hour. Effects may lasts for 3–4 days
- CVS: Vasodilation and fall in BP, but tachycardia increase CO
- CNS: Sedation. Rapid infusion can cause seizures
