Category Archives: Fluid and Electrolyte Imbalances
BALANCED SALT SOLUTIONS
- Intravenous “balanced” solutions include crystalloids and colloids with minimal effect on the homeostasis of the extracellular compartment, and in particular on acid–base equilibrium and electrolyte concentrations. These are fluids which are able to leave the plasma pH unchanged after its administration.
- There are two main categories of balanced solutions : (1) fluids causing a minimal effect on acid–base equilibrium, having an electrolyte content with an in vivo strong ion difference (SID), i.e., the SID after metabolism of the organic anion, close to 24–29 mEq/L; (2) fluids having a normal or sub-normal Cl−content(Cl− ≤ 110 mEq/L).
- The ideal balanced solution should have an in vivo SID equal to the baseline concentration of HCO3−. If the SID of the infused fluid is greater than plasma HCO3−, plasma pH will tend toward alkalosis; if the SID of the infused fluid is lower than plasma HCO3−, plasma pH will tend toward acidosis, as it is always the case for NaCl 0.9%.
- An isotonic balanced solution leaving unaltered acid–base equilibrium (i.e., with an SID close to 24 mEq/L) will necessarily have a Cl− content > 110 mEq/L (as in Sterofundin-ISO).
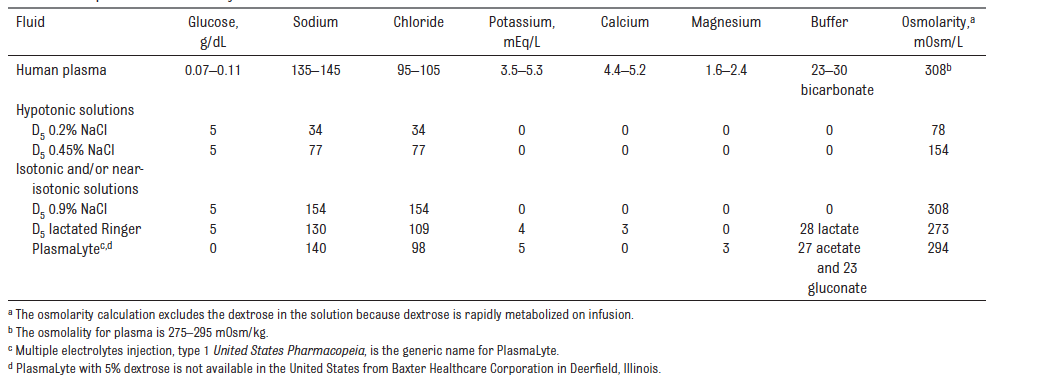
- In contrast, a fluid with an SID of 24 mEq/L and a lower Cl−content will necessarily be slightly hypotonic (as with Lactated Ringer’s). Finally, an isotonic fluid with a low Cl−content will necessarily have a higher SID (as with PlasmaLyte), with a consequent alkalizing effect.
- Chloride-rich NaCl 0.9% causes a higher dose-dependent degree of acidosis and hyperchloremia, which possibly favors the contraction of vascular smooth muscles, potentially leading to a reduced renal perfusion.
- Hyperchloremia may cause increased tubule-glomerular feedback and decreased renal cortical perfusion. NaCl 0.9%, being slightly hypertonic, likely causes an increased incretion of arginine vasopressin.
- These effects can conceivably contribute to the slower renal excretion of NaCl 0.9% as compared to balanced solutions. Indeed, more fluid will be retained in the interstitial space, with the consequent propensity to cause more edema.
- Therefore, the use of balanced solutions, particularly in patients that potentially need a significant amount of intravenous fluids, seems to be a reasonable pragmatic choice.
- On the contrary, saline may be an intuitive choice for patients with hypovolemic hyponatremia or hypochloremic metabolic alkalosis.
- In any other settings, the most important reason to choose NaCl 0.9% over balanced solutions is likely economic in nature. Therefore, the patient’s serum chloremia is an important factor to determine the appropriate type of fluids
HYPONATRAEMIA CORRECTION 2020 UPDATES
VIVA AID: INTRAVENOUS FLUIDS IN PAEDIATRIC POPULATION; SALIENT POINTS FROM VARIOUS GUIDELINES
NICE 2015 GUIDELINES
- For fluid resuscitation in children and young people: use glucose‑free crystalloids that contain sodium in the range 131–154 mmol/litre, with a bolus of 20 ml/kg over less than 10 minutes. Take into account pre‑existing conditions like cardiac disease or kidney disease, as smaller fluid volumes may be needed.
- For term neonates who need IV fluid resuscitation: use glucose‑free crystalloids that contain sodium in the range 131–154 mmol/litre, with a bolus of 10–20 ml/kg over less than 10 minutes.
- Do not use tetrastarch for fluid resuscitation.
- Calculate routine maintenance IV fluid rates for children and young people using the Holliday–Segar formula (100 ml/kg/day for the first 10 kg of weight, 50 ml/kg/day for the next 10 kg and 20 ml/kg/day for the weight over 20 kg). Be aware that over a 24‑hour period, males rarely need more than 2500 ml and females rarely need more than 2000 ml of fluids.
- Calculate routine maintenance IV fluid rates for term neonates according to their age, using the following as a guide:
- From birth to day 1: 50–60 ml/kg/day.
- Day 2: 70–80 ml/kg/day.
- Day 3: 80–100 ml/kg/day.
- Day 4: 100–120 ml/kg/day.
- Days 5–28: 120–150 ml/kg/day.
- IV fluids for routine maintenance in children and young people: initially use isotonic crystalloids that contain sodium in the range 131–154 mmol/litre.
- Measure plasma electrolyte concentrations and blood glucose when starting IV fluids for routine maintenance (except before most elective surgery), and at least every 24 hours thereafter.
- Base any subsequent IV fluid prescriptions on the plasma electrolyte concentrations and blood glucose measurements.
- If term neonates need IV fluids for routine maintenance: initially use isotonic crystalloids that contain sodium in the range 131–154 mmol/litre with 5–10% glucose
- If there is a risk of water retention associated with non‑osmotic antidiuretic hormone (ADH) secretion, consider either:
- restricting fluids to 50–80% of routine maintenance needs or
- reducing fluids, calculated on the basis of insensible losses within the range 300–400 ml/m2/24 hours plus urinary output.
EUROPEAN CONSENSUS 2011 FOR INTRAOPERATIVE FLUID THERAPY
An appropriate solution for intraoperative infusion in children should have an osmolarity and sodium content close to the physiologic range in order to avoid hyponatraemia, an addition of 1–2.5% glucose in order to avoid hypoglycaemia, lipolysis or hyperglycaemia and should also include metabolic anions (i.e. acetate, lactate or malate) as bicarbonate precursors to avoid acid–base balance disturbances (i.e. hyperchloraemic acidosis). The intraoperative infusion of isotonic solutions containing 1–2.5% glucose in children is considered well established use in Europe
BELGIAN PERIOPERATIVE FLUID RECOMMENDATIONS 2012
For children undergoing uncomplicated day-case surgery or minor surgery and those expected to remain nil-by-mouth for at least 24 hours after surgery or undergoing major surgery, a full volume maintenance fluid should be administered during the intraoperative period and immediate post-operative period, as this is associated both with a reduced incidence of postoperative nausea and vomiting particularly in those children receiving opioids, and with a significantly reduced postoperative increase in ADH concentration. The latter presumed to be a result of correction of hypovolemia.
During the first postoperative day, decreased volumes of the maintenance fluid consisting of an isotonic solution at two-thirds or 70% of the calculated maintenance rate is recommended, provided the child is normovolemic.
This solution would preferably be enriched with glucose 5% (50 ml glucose 50% in 500 ml fluid) in order to provide an adequate caloric supply as recommended (4 to 8 mg glucose/kg/min). In addition, the osmolarity of such a solution makes it possible to be administered on a peripheral venous access.
Recognizing that fluids used to replace ongoing losses should reflect the electrolyte composition of fluid lost, NaCl 0.9% has been considered as appropriate in most cases. Isotonic fluids including colloids are to be used as a bolus in the event of hypovolemia.
Consider iv. fluids as medications.
Administer isotonic fluids (saline 0.9%, Plasmalyte®, Hartmann® or colloids) as a bolus in the event of hypovolemia.
Monitoring plasma electrolytes and glucose concentrations regularly i.e. once daily or more if clinically indicated (documented plasma [Na] < 135 mmol/L)
AMERICAN ACADEMY OF PAEDIATRICS 2018
The American Academy of Pediatrics recommends that patients 28 days to 18 years of age requiring maintenance IVFs should receive isotonic solutions with appropriate potassium chloride and dextrose because they significantly decrease the risk of developing hyponatremia. (For the purposes of this guideline, isotonic solutions have a sodium concentration similar to PlasmaLyte, or 0.9% NaCl)
APA CONSENSUS GUIDELINE ON PERIOPERATIVE FLUID MANAGEMENT IN CHILDREN 2007/ 2010 REVIEW
EXECUTIVE SUMMARY
1. Children can safely be allowed clear fluids 2 hours before surgery without increasing the risk of aspiration.
2. Food should normally be withheld for 6 hours prior to surgery in children aged 6 months or older.
3. In children under 6 months of age it is probably safe to allow a breast milk feed up to 4 hours before surgery
4. Dehydration without signs of hypovolaemia should be corrected slowly.
5. Hypovolaemia should be corrected rapidly to maintain cardiac output and organ perfusion.
6. In the child, a fall in blood pressure is a late sign of hypovolaemia.
7. Maintenance fluid requirements should be calculated using the formula of Holliday and Segar
8. A fluid management plan for any child should address 3 key issues
i. any fluid deficit which is present
ii. maintenance fluid requirements
iii. any losses due to surgery e.g. blood loss, 3rd space losses
9. During surgery all of these requirements should be managed by giving isotonic fluid in all children over 1 month of age
10. The majority of children over 1 month of age will maintain a normal blood sugar if given non-dextrose containing fluid during surgery
11. Children at risk of hypoglycaemia if non-dextrose containing fluid is given are those on parenteral nutrition or a dextrose containing solution prior to theatre, children of low body weight (<3rd centile) or having surgery of more than 3 hours duration and children having extensive regional anaesthesia. These children at risk should be given dextrose containing solutions or have their blood glucose monitored during surgery.
12. Blood loss during surgery should be replaced initially with crystalloid or colloid, and then with blood once the haematocrit has fallen to 25%. Children with cyanotic congenital heart disease and neonates may need a higher haematocrit to maintain oxygenation.
13. Fluid therapy should be monitored by daily electrolyte estimation, use of a fluid input/output chart and daily weighing if feasible.
14. Acute dilutional hyponatraemia is a medical emergency and should be managed in PICU.
