🍃Ventilatory responses to hypoxia and hypercapnia are impaired secondary to reduced central nervous system activity.
🍃The respiratory depressant effects of benzodiazepines, opioids, and volatile anesthetics are exaggerated.
🍃These changes compromise the usual protective responses against hypoxemia after anesthesia and surgery in elderly patients.
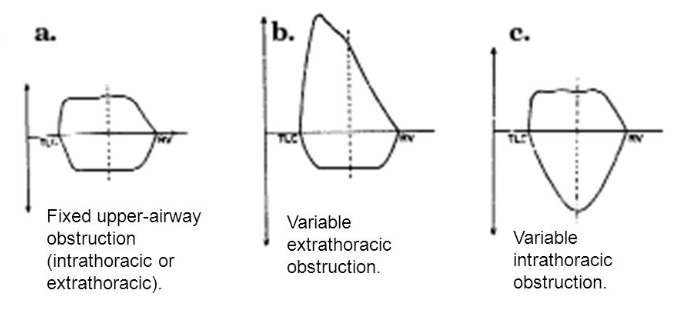
🍃The loss of elastic recoil combined with altered surfactant production leads to an increase in lung compliance.
🍃Increased compliance leads to limited maximal expiratory flow and a decreased ventilatory response to exercise.
🍃Loss of elastic elements within the lung is associated with enlargement of the respiratory bronchioles and alveolar ducts, and a tendency for early collapse of the small airways on exhalation.
🍃There also is a progressive loss of alveolar surface area secondary to increases in size of the interalveolar pores of Kohn. This results in increased anatomic dead space, decreased diffusing capacity, and increased closing capacity all leading to impaired gas exchange.
🍃Loss of height and calcification of the vertebral column and rib cage lead to a typical barrel chest appearance with diaphragmatic flattening.
🍃The flattened diaphragm is mechanically less efficient, and function is impaired further by a significant loss of muscle mass associated with aging. Functionally, the chest wall becomes less compliant, and work of breathing is increased.
🍃Total lung capacity is relatively unchanged.
🍃Residual volume increases by 5% to 10% per decade.
🍃Vital capacity decreases.
🍃Closing capacity increases with age.
🍃Functional residual capacity (FRC) is determined by the balance between the inward recoil of the lungs and the outward recoil of the chest wall. FRC increases by 1%–3% per decade because at relaxed end expiration, the rate of decrease in lung recoil with aging exceeds that of the rate of increase in chest wall stiffness.
🍃In younger individuals, closing capacity is below functional residual capacity. At 44 years of age, closing capacity equals functional residual capacity in the supine position, and at 66 years of age, closing capacity equals functional residual capacity in the upright position.
🍃When closing capacity encroaches on tidal breathing, ventilation-perfusion mismatch occurs.
🍃When functional residual capacity is below closing capacity, shunt increases, and arterial oxygenation decreases. This results in impairment of preoxygenation. Increased closing capacity in concert with depletion of muscle mass causes a progressive decrease in forced expiratory volume in 1 second by 6% to 8% per decade.
🍃Increases in pulmonary vascular resistance and pulmonary arterial pressure occur with age and may be secondary to decreases in cross-sectional area of the pulmonary capillary bed. Hypoxic pulmonary vasoconstriction is blunted in elderly individuals and may cause difficulty with one-lung ventilation.
Ref: Geriatric Anesthesia 2/e , Miller’s Anesthesia 7/e
#Physiology , #Anesthesia , #Geriatrics