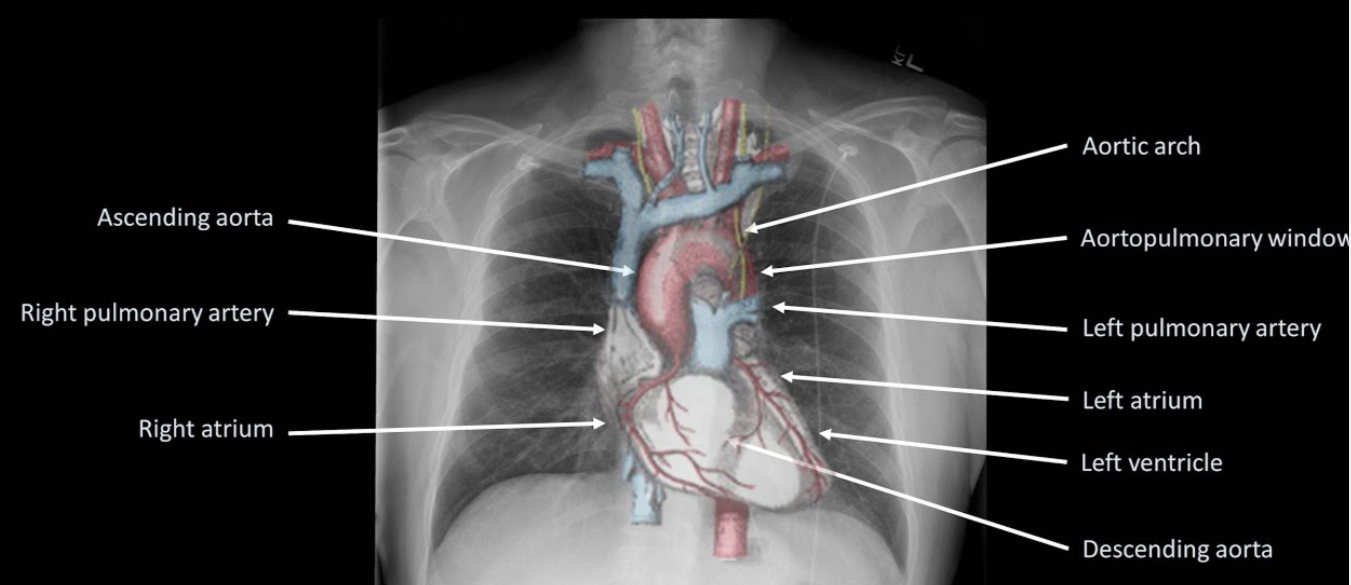
A postero-anterior (PA) projectionn will not produce as much magnification of the heart and mediastinum as an antero-posterior (AP) projection. So PA films are the preferred ones. Here the scapula is rotated; so the lung fields are clear.
A PA film is taken with the film cassette in front of the patient and the beam delivered from behind with the patient in an upright position.
Portable films and those taken in ICUs are all AP projection. All anterior structures appear magnified—heart, mediastinum, sternum, clavicles, and ribs
The supine position causes distension of the upper lobe blood vessels, which may be confused with elevated left atrial pressure
A lateral X-ray is useful in viewing retrosternal and chest wall lesions, localising lesions in the AP dimension, locate lesions behind the left side of the heart or in the posterior recesses of the lungs. Lateral decubitus—used in diagnosing very small collection of air or fluid in the pleural space.
A left lateral (with the left side of the chest against the film and the beam projected from the right) is the standard projection.
The heart is magnified less with a left lateral as it is closer to the film.
To visualize lesions in the left hemithorax, obtain a left lateral film and for right-sided lesions a right lateral.
Expiratory films are used to assess air trapping in bronchial obstruction such as a foreign body.
A pneumothorax always appears larger on an expiratory film and occasionally a small pneumothorax may only be visible on expiration.
Films if accidentally taken in expiration, can result in spurious magnifcation of the heart and mediastinum.
- PROJECTION: The different projections of importance to us are Postero Anterior (PA), Antero Posterior (AP), Lateral, Supine, and Lateral decubitus.
- ROTATION: An image is not rotated if the clavicular heads are equidistant to the
corresponding thoracic spine
- INSPIRATION: An inspiratory picture shows a ‘lot of lung’. In inspiratory films the
level of the diaphragm is at the level of ribs 5/6 anteriorly and 8/10
posteriorly. (AR6PR10)
- PENETRATION: A film is adequately penetrated if the vertebral bodies can be
visualised against the cardiac silhouette
A normal chest radiograph can be summarised as ‘…the trachea is central and the hila are normal. Lung fields are clear with no air or fluid collection. Heart and mediastinum appear normal and not displaced. There is no free air under the diaphragm, and the angles are clear. Also, the bones and soft tissues appear normal…’
–>Before diagnosing a CXR as normal, look at the areas where
pathology is commonly missed.
*Apices (including behind the 1st rib and clavicle)—small pneumothoraces and masses
*Hila—masses and lymph nodes; left hilum is 1–2 cm higher than right
*Behind the heart—left lower lobar collapse and hiatus hernia
*Below the diaphragm—free gas
*Soft tissues—breast shadow or absence (look for lung and bone metastasis)
#xray ,#radiology ,#imaging , #XrayBasics , #anaesthesia
Reference: Radiology for Anaesthesia and Intensive Care (Richard Hopkins, Carol Peden and Sanjay Gandhi)