DEFINITION:
-
Pain is ‘an unpleasant sensory and emotional experience associated with actual or potential tissue damage’. (IASP: International Association for the Study of Pain)
CLASSIFICATION:
According to chronicity
- Acute: Recent onset pain with identifiable cause
- Chronic: Pain persisting beyond the time of injury or healing without definable cause
According to nature
Nociceptive pain: Pain occurring due to stimulation of peripheral sensory nerve fibres (nociceptors) that respond to potentially harmful stimuli; further divided into
- Superficial and Deep somatic pain: Relatively well localized pain due to activation of peripheral nociceptors.
- Visceral pain (organs, viscera) – Diffuse pain that may be difficult to localize or referred to a superficial structure which is usually distant to the source of the pain
Neuropathic pain: Pain that occurs due to a primary lesion or dysfunction in the nervous system itself.
THE GATE CONTROL THEORY OF PAIN:
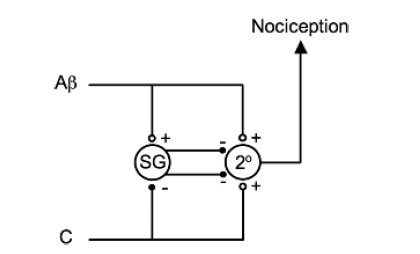
- Melzack and Wall theorized that the transmission of a peripheral painful stimulus to the CNS occurs via a gate at spinal cord level. This gate comprises an inhibitory interneurone in the substantia gelatinosa that may be either stimulated or inhibited by different afferent inputs.
-
The Aβ fibres are examples of afferents that stimulate inhibitory interneurones (in the substantia gelatinosa (SG)) and, therefore, prevent nociceptive transmission to the CNS. The C fibres are examples of afferents that inhibit inhibitory interneurones and, therefore, enhance nociceptive transmission. Note that both types of fibres stimulate the second-order neurone (2°) directly but it is the interneurone that modifies the transmission.
-
Laminae 2 & 3 are called the substantia gelatinosa and is the site of the ‘gate control theory’ of pain.
PAIN PATHWAY
-
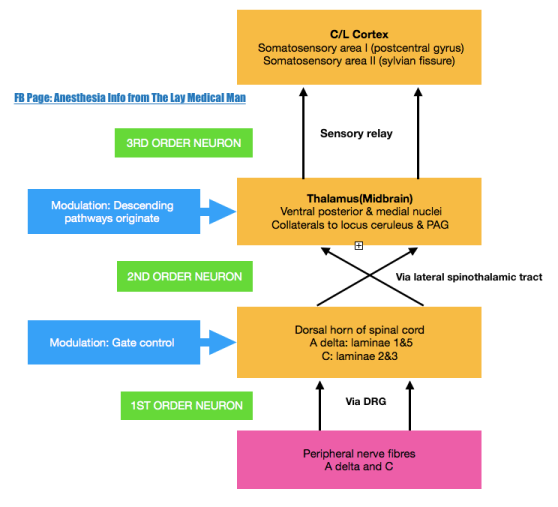
There are three levels of neuronal involvement and the signals may be modulated at two points during their course to the cerebral cortex. Descending inhibitory pathways arise in the midbrain and pass to the dorsal horn. Multiple different neurotransmitters are involved in the pathway and include GABA,NMDA, noradrenaline and opioids.
-
Noxious stimuli –>tissue damage –>mediators–> nociceptors stimulation–> action potential –> propagated along afferent nerve fibres C & Aδ –> dorsal horn of the spinal cord –> Synaptic transmission with secondary interneurones occurs in Rexed’s laminae –> secondary interneurones decussate and travel in the anterolateral spinothalamic tracts –> through the brainstem –>to the thalamus –> tertiary afferents project to the somatosensory cortex.
-
Some spinal ascending fibres transmit impulses to the reticular-activating system, and to higher centres involved with affect, emotion and memory.
-
Descending fibres from cortex, thalamus and brainstem exert an inhibitory influence on pain transmission in the dorsal horn
-
An immediate polysynaptic withdrawal reflex occurs at the level of the spinal cord as some interneurones connect to motor neurones at many levels. This is a protective reflex.
DESCENDING INHIBITORY PATHWAYS
-
Periaqueductal grey (PAG) in the midbrain receives projections from the thalamus, hypothalamus, amygdala and cortex, and delivers projections to the nucleus raphe magnus (NRM) in the medulla, whose fibres synapse in the substantia gelatinosa of the dorsal horn. Its transmitters include endorphins and enkephalins (MOP opioid receptors) and serotonin (5HT1 and 5HT3 receptors).
-
Locus caeruleus (LC) is an important brainstem nucleus projecting descending inhibitory pathways to the dorsal horn via noradrenaline (α-adrenergic receptors).
