- NIV is a technique of providing ventilation without the use of an artificial airway.
- NIV has two primary pressure settings
-
The inspiratory positive airway pressure (IPAP) is similar to the peak airway pressure in traditional mechanical ventilation. A higher IPAP level would result in a larger tidal volume and minute ventilation.
-
The expiratory positive airway pressure (EPAP) is the same as PEEP during mechanical ventilation or CPAP during spontaneous breathing. In addition to its ability to improve oxygenation by increasing the functional residual capacity, EPAP also relieves upper airway obstruction with its splinting action.
-
SpO2, Capnography, PaO2, PaCO2 etc may be used for the titration of appropriate IPAP and EPAP levels.
-
CPAP (Continuous positive airway pressure) provides positive airway pressure during spontaneous breaths and it does not include any mechanical breaths. For this reason, the work of breathing is entirely assumed by the patient. CPAP is active when IPAP=EPAP. CPAP is the treatment of choice for obstructive sleep apnea without significant carbon dioxide retention. CPAP should not be used in apnea due to neuromuscular causes, if there is progressive hypoventilation or facial trauma
-
Bilevel PAP (Bilevel positive airway pressure) provides IPAP which controls peak inspiratory pressure during inspiration and EPAP that controls end-expiratory pressure. Indications are acute respiratory failure and acute hypercapnic exacerbations of COPD
-
In patients with acute cardiogenic pulmonary edema, CPAP or bilevel PAP ventilation has been found to reduce the need for subsequent mechanical ventilation
-
Inability to protect the airway from secretions or aspiration, apnoea, facial trauma are contraindications for NPPV.
- We can use nasal or oronasal mask as the interface for delivering NIV
Monthly Archives: September 2019
VIVA SCENE: SUBCUTANEOUS EMPHYSEMA – RADIOLOGY
Subcutaneous emphysema, refers to gas in the subcutaneous tissues
Clinically it is felt as crepitus
In the trauma situation, its presence indicates possible serious injuries that do require urgent management.
RADIOGRAPHY
CHEST X-RAY
There are often striated lucencies in the soft tissues that may outline muscle fibers. It can outline the pectoralis major, giving rise to the ginkgo leaf sign. Often there are displaced rib fractures indicating a cause of the gas.
CT
Subcutaneous emphysema is visible on CT scans, with pockets of gas seen as extremely dark low attenuation areas in the subcutaneous space.
USG
Well defined comet tail artefacts can be seen
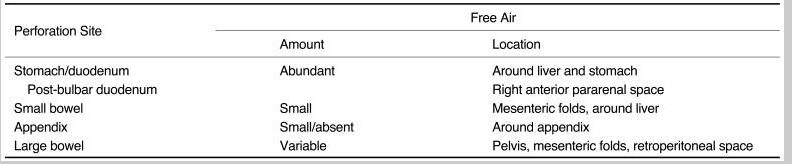
VIVA SCENE: CT ABDOMEN SHOWING FREE AIR
- The diagnosis of GI tract perforation is based on the direct CT findings, such as discontinuity of the bowel wall and the presence of extraluminal air, and on the indirect CT findings, such as bowel wall thickening, abnormal bowel wall enhancement, abscess and an inflammatory mass adjacent to the bowel
- The air may not be contained within any visible bowel wall.
- Direct visualization of the discontinuity of the bowel wall can specify the presence and site of GI tract perforation, which is marked by a low-attenuating cleft that usually runs perpendicular to the bowel wall on CT
- The falciform ligament may become outlined with air in a supine patient with free abdominal gas.

VIVA SCENE: ADH- MECHANISM OF ACTION; ANALOGUES ; EFFECTS
MECHANISM OF ACTION:
- Anti Diuretic Hormone (ADH) stimulates V2 receptors on collecting ducts, which increases adenylate cyclase activity. This causes fusion of pre-formed water channels on the apical membrane resulting in increased permeability of the collecting ducts to water.
ADH is secreted in response to:
- Hyperosmolarity: detected by osmoreceptors in the hypothalamus, outside the blood–brain barrier. Osmoreceptors then stimulate thirst
Volume depletion (ECF) detected by low-pressure baroreceptors in great veins, atria and pulmonary vessels, and high-pressure baroreceptors in the carotid sinus and aortic arch
Angiotensin II (AGII)
- Other: pain, exercise, stress, emotion, nausea and vomiting, standing, nicotine, morphine, barbiturates, carbamazepine.
EFFECTS:
It regulates Total Body Water (TBW).
The specific renal effects of ADH on water balance include:
- Increased water permeability in cortical collecting tubule (V2 receptors)
- Increased water and urea permeability in medullary collecting tubule
- Increased retention of water
- Reduced urine volume
OTHER EFFECTS
- It stimulates thirst
- Release of factor VIII by the endothelium
- Platelet aggregation and degranulation
- Arteriolar vasoconstriction
- Glycogenolysis in the liver
- Brain neurotransmitter
- Secretion of ACTH from the anterior pituitary gland.

VASOPRESSIN RECEPTOR AGONISTS
Arginine-Vasopressin: A V receptor agonist is a potent alternative to vasoconstrictors in the treatment of fluid and catecholamine-refractory septic shock
Terlipressin is a selective V1 receptor agonist and may be more potent than arginine-vasopressin in restoring catecholamine refractory septic shock
Desmopressin (1-deamino-8-D-arginine vasopressin) is a synthetic vasopressin analog, that acts as an agonist at V1B and V2 receptors. Exhibits antidiuretic and haemostatic properties. So also used in the management of some forms of hemophilia and von Willebrand’s disease


ANTAGONISTS
Vaptans act by inhibiting vasopressin’s action on all the 3 types of receptors. e.g. Conivaptan (unselective), Tolvaptan (V2 selective). Used in the treatment of euvolemic (eg SIADH) and hypervolemic (CHF) hyponatremias, nehrogenic DI, cirrhosis, PCKD etc
VIVA SCENE: HYPOCALCAEMIA
Plasma calcium < 2.2 mmol/L
Normal values: Total calcium 2.25-2.60 mmol/L; ionised calcium 1.12-1.32 mmol/L
HYPOCALCAEMIA CAUSES:
-
Decreased parathyroid hormone
-
Decreased Vitamin D activity (e.g. intestinal malabsorption, liver disease, CRF)
-
Increased calcium loss (e.g. chelating agents, calcification of soft tissues)
-
Decreased ionised calcium (e.g. alkalosis)
- Tumour Lysis Syndrome
- Diarrhoea, vomiting, and nasogastric suction can cause hypomagnesaemia with secondary hypocalcaemia (HSH)
CLINICAL FEATURES:
- Tetany
- Seizures
- Emotional instability/agitation/anxiety
- Myopathy
ECG:
-
QTc prolongation by prolonging the ST segment
-
Torsades de pointes and atrial fibrillation in severe cases
NB: The corrected QT interval (QTc) is taken as the time between the beginning of the QRS complex and the end of the T wave, it is less than 440 ms in men and 460 ms in women. Severe hypocalcaemia (less than 1.9 mmol/L) may cause a prolongation of the QTc. A QTc greater than 500 ms is associated with an increased risk of Torsades de Pointes.
TREATMENT:
- Ca2+ 0.5mL/kg (max 20mL) of 10% calcium gluconate OR 0.2mL/kg of 10% calcium chloride
- Administer by slow IV (max 2 mL/min), repeat if necessary.
- Calcium can precipitate or exacerbate digitalis toxicity therefore IV calcium must be given very slowly in patients on digoxin and the ECG must be monitored continuously
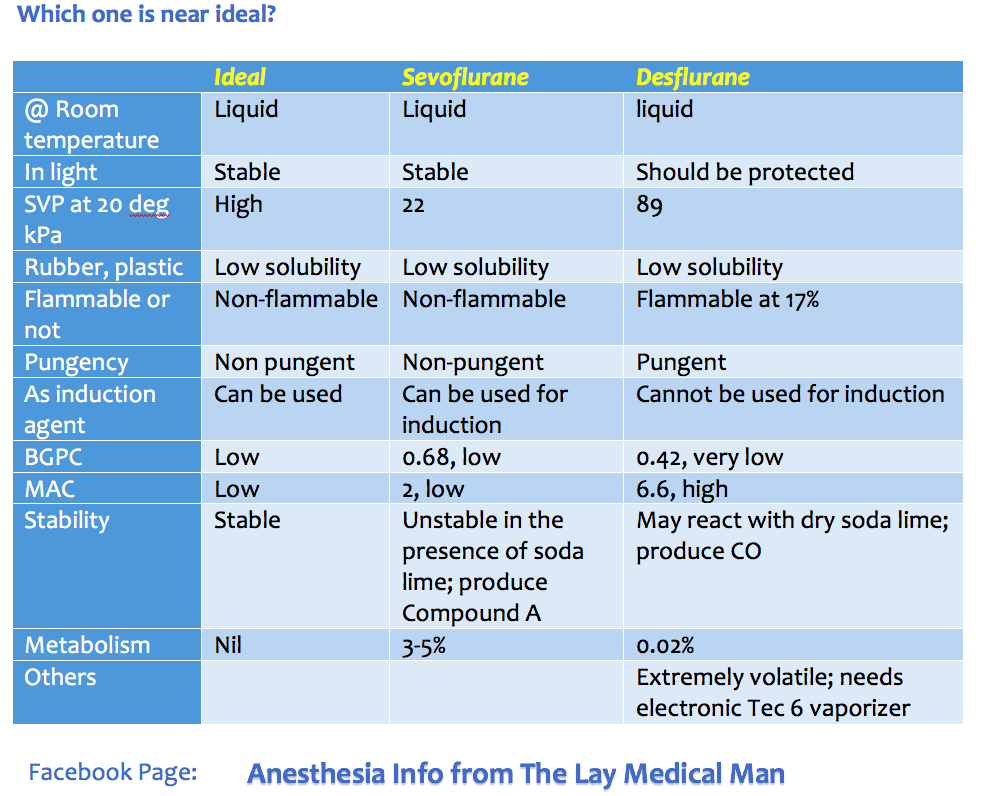
VIVA SCENE: DESFLURANE
- Desflurane is a fluorinated methyl ethyl ether (MW = 168)
- Its an irritant gas, so cannot be used for induction
- MAC is 6.6% ( for an infant the MAC raises to 9.4%)
- Boiling point is low at 22.8 degrees compared to other agents
- SVP at 20 degrees is very high at 89.2 compared to other agents
- Extremely volatile; so needs an electronic Tec 6 vaporizer
- Has a low OGPC of 29 = potency is low
- Has a high BGPC of 0.42 = rapid onset and offset
- Only 0.02% of desflurane will get metabolised (to trifluoroacetic acid)
- Its effect on the CVS is modest: reduce SVR only above 2.2 MAC and effect on contractility is less than other agents. It increases HR like isoflurane
- Like other agents it reduces TV and increases RR
- Like other agents, it has the potential to increase cerebral blood flow above 1 MAC
- With dry sodalime, it has the potential to react and produce carbon monoxide
VIVA SCENE: RADIAL NERVE COURSE AND CAUSES OF INJURY
COURSE:
- The radial nerve (C5–8, T1) transmits fibres from all the roots of the brachial plexus.
- At its origin it lies behind the third part of the axillary artery; it then passes between the long and medial heads of triceps into the posterior compartment of the arm, accompanied by the profunda branches of the brachial vessels.
- It descends first along the spiral groove of humerus, and then between muscle planes
- A hand’s breadth above the elbow, the nerve reaches the lateral margin of the humerus, and enters once more into the anterior compartment of the arm, where it lies between brachialis and brachioradialis. At this point, the nerve is susceptible to compression injury, in particular from an arterial tourniquet placed too low around the arm.
- It ends in front of the lateral epicondyle of the humerus by dividing into two terminal branches, the superficial radial nerve and the posterior interosseous nerve.
BRANCHES:
The muscular branches:
- Medial group (arising in the axilla): Supplies: a long head of triceps b medial head of triceps.
- Posterior group (arising in the spiral groove) : a medial head of triceps b lateral head of triceps c anconeus.
- Lateral group: a brachialis (together with musculocutaneous nerve) b brachioradialis c extensor carpi radialis longus
The cutaneous branches:
- The posterior cutaneous nerve of the arm, which arises in the axilla and supplies the skin over the proximal one-third of the posterior aspect of the arm.
- The posterior cutaneous nerve of the forearm, which arises in the spiral groove, supplies the skin over the posterolateral aspect of the forearm.
- The lower lateral cutaneous nerve of the arm, supplies an area of skin over the lateral aspect of the arm just above the elbow.
The posterior interosseous nerve (terminal branch), passes into the posterior compartment of the forearm. It supplies supinator, many extensors and abductor pollicis longus. It also supplies the wrist joint.
The superficial radial nerve (terminal branch) is entirely sensory. It divides into dorsal digital nerves and supply the dorsal aspect of the hand upto the radial half of the ring finger.
CAUSES OF RADIAL NERVE INJURY:
- Saturday Night Palsy: Caused by prolonged compression of the nerve at the spiral groove.
- Mechanical compression of the radial nerve in the spiral groove can also occur as a result of the continuous use of crutches or prolonged kneeling in a “shooting” position
- As a delayed complication of a chronic intramuscular injection leading to muscle fibrosis
- From prolonged inflation of an automatic blood pressure cuff especially when placed over the distal third around the arm, in a lean patient. Here, the radial nerve lies in direct contact with the humerus and there are no muscle fibers to act as a cushion between the nerve and the periosteum of the bone
- Humeral shaft fracture
VIVA SCENE: PAIN: Most important points summarised
DEFINITION:
-
Pain is ‘an unpleasant sensory and emotional experience associated with actual or potential tissue damage’. (IASP: International Association for the Study of Pain)
CLASSIFICATION:
According to chronicity
- Acute: Recent onset pain with identifiable cause
- Chronic: Pain persisting beyond the time of injury or healing without definable cause
According to nature
Nociceptive pain: Pain occurring due to stimulation of peripheral sensory nerve fibres (nociceptors) that respond to potentially harmful stimuli; further divided into
- Superficial and Deep somatic pain: Relatively well localized pain due to activation of peripheral nociceptors.
- Visceral pain (organs, viscera) – Diffuse pain that may be difficult to localize or referred to a superficial structure which is usually distant to the source of the pain
Neuropathic pain: Pain that occurs due to a primary lesion or dysfunction in the nervous system itself.
THE GATE CONTROL THEORY OF PAIN:
- Melzack and Wall theorized that the transmission of a peripheral painful stimulus to the CNS occurs via a gate at spinal cord level. This gate comprises an inhibitory interneurone in the substantia gelatinosa that may be either stimulated or inhibited by different afferent inputs.
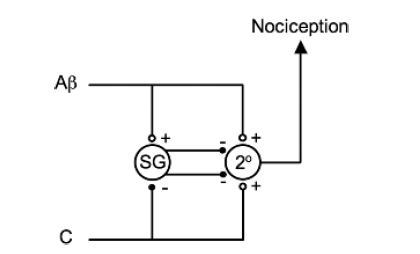
-
The Aβ fibres are examples of afferents that stimulate inhibitory interneurones (in the substantia gelatinosa (SG)) and, therefore, prevent nociceptive transmission to the CNS. The C fibres are examples of afferents that inhibit inhibitory interneurones and, therefore, enhance nociceptive transmission. Note that both types of fibres stimulate the second-order neurone (2°) directly but it is the interneurone that modifies the transmission.
-
Laminae 2 & 3 are called the substantia gelatinosa and is the site of the ‘gate control theory’ of pain.
PAIN PATHWAY
-
There are three levels of neuronal involvement and the signals may be modulated at two points during their course to the cerebral cortex. Descending inhibitory pathways arise in the midbrain and pass to the dorsal horn. Multiple different neurotransmitters are involved in the pathway and include GABA,NMDA, noradrenaline and opioids.
-
Noxious stimuli –>tissue damage –>mediators–> nociceptors stimulation–> action potential –> propagated along afferent nerve fibres C & Aδ –> dorsal horn of the spinal cord –> Synaptic transmission with secondary interneurones occurs in Rexed’s laminae –> secondary interneurones decussate and travel in the anterolateral spinothalamic tracts –> through the brainstem –>to the thalamus –> tertiary afferents project to the somatosensory cortex.
-
Some spinal ascending fibres transmit impulses to the reticular-activating system, and to higher centres involved with affect, emotion and memory.
-
Descending fibres from cortex, thalamus and brainstem exert an inhibitory influence on pain transmission in the dorsal horn
-
An immediate polysynaptic withdrawal reflex occurs at the level of the spinal cord as some interneurones connect to motor neurones at many levels. This is a protective reflex.
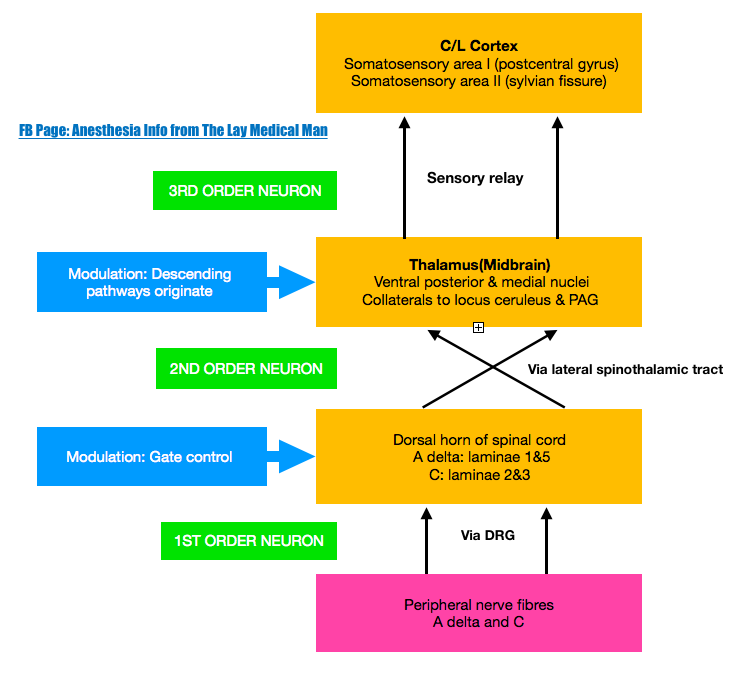
DESCENDING INHIBITORY PATHWAYS
-
Periaqueductal grey (PAG) in the midbrain receives projections from the thalamus, hypothalamus, amygdala and cortex, and delivers projections to the nucleus raphe magnus (NRM) in the medulla, whose fibres synapse in the substantia gelatinosa of the dorsal horn. Its transmitters include endorphins and enkephalins (MOP opioid receptors) and serotonin (5HT1 and 5HT3 receptors).
-
Locus caeruleus (LC) is an important brainstem nucleus projecting descending inhibitory pathways to the dorsal horn via noradrenaline (α-adrenergic receptors).
VIVA SCENE: PARACETAMOL Vs MORPHINE CENTRAL MOA
PARACETAMOL:
Central action via COX 3 inhibition which is associated with decreased brain PGE2 levels. It also modulates endogenous cannabinoid system
MORPHINE:
Morphine work by stimulating presynaptic Gi-protein-coupled MOP and KOP opioid receptors. Binding of the ligand causes the following events:
> Closure of voltage-gated Ca2+ channels
> Decreased cAMP production
> Stimulation of K+ efflux from the cell
> Hyperpolarisation of the cell membrane.
> This leads to decreased excitability of the cell and therefore decreased neurotransmitter release and pain transmission
VIVA SCENE: Ideal Inhalational Agent