COMPATIBILITY: RBC TRANSFUSION
In red cell transfusion, there must be ABO and RhD compatibility between the donor’s red cells and the recipient’s plasma.
All healthy normal adults of group A, group B and group O have ANTIBODIES IN THEIR PLASMA against the red cell types (antigens) that they have not inherited
Among the ABO blood groups:
Group A individuals have antibody to group B
Group B individuals have antibody to group A
Group O individuals have antibody to group A and group B
Group AB individuals do not have antibody to group A or B. So,
1 Group O individuals can receive blood from group O donors only ( as the antibodies against A or B in their plasma will react with any A or B antigens which enter the circulation)
2 Group A individuals can receive blood from group A and O donors
3 Group B individuals can receive blood from group B and O donors
4 Group AB individuals can receive blood from AB donors, and also from group A, B and O donors ( as their plasma don’t have any antibodies against any antigens)
RhD RED CELL ANTIGENS AND ANTIBODIES
Is the second most important group system. Out of the existing C,D and E antigens, D is the most antigenic one. Anti D antibodies are not normally found in the blood of Rh negative individuals; instead they develop it only when itcomes into contact with Rh positive blood during child birth or inappropriate transfusion. In case of subsequent transfusins or pregnancies with Rh positive blood- this can cause rapid destruction of RhD positive red cells (Hemolytic disease of the newborn[HDN] in subsequent pregnancies; to prevent this sensitization we should give Rhesus imunoglobulin= Anti-D prophylaxis- to the Rh negative mother who gave birth to an Rh positive baby). The fetal red cells are haemolysed, causing severe anaemia. HDN due to ABO incompatibility is usually less severe than Rh incompatibility.). FFP does not need to be Rh-compatible. Anti-D prophylaxis is not necessary in Rh D-negative recipients of Rh D-positive FFP.
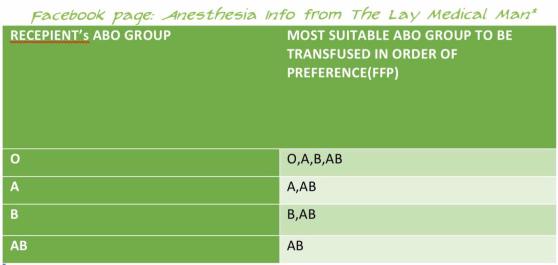
PLASMA TRANSFUSION: COMPATIBILITY
In plasma transfusion, group AB plasma can be given to a patient of any ABO group because it contains neither anti-A nor anti-B antibody.
1 Group AB plasma (no antibodies) can be given to any ABO group patients
2 Group A plasma (anti-B) can be given to group O and A patients
3 Group B plasma (anti-A) can be given to group O and B patients
4 Group O plasma (anti-A + anti-B) can be given to group O patients only
FFP does not need to be Rh-compatible (However, the unit will still be labelled as Rh +ve or Rh −ve) ; anti-D prophylaxis is not necessary in Rh D-negative recipients of Rh D-positive FFP
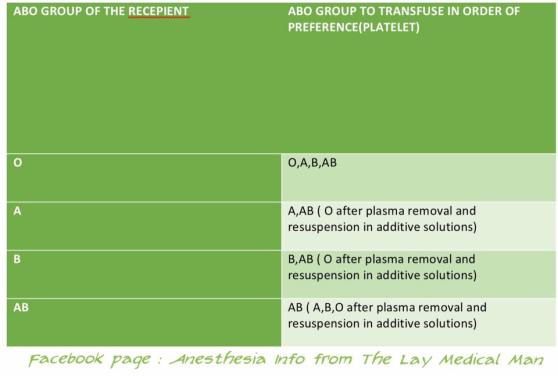
PLATELET TRANSFUSION: COMPATIBILITY
The Platelet Concentrates( PCs ) transfused must be ABO-identical, or at least ABO-compatible, in order to give a good yield ( Ideally, ABO identical units should be used but, in an emergency, ABO non-identical units can be used, although the improvement seen in platelet count post-transfusion may be less.)
Group O PC can be used for patients with blood groups A, B, and AB ONLY IF, they are resuspended in additive/preservative solutions, or if negative for high titre anti-A/A,B
ABO-incompatible PCs have reduced efficacy and, preferably, should not be used
Rh-negative patients, in particular women of childbearing age, should receive, if possible, RhD-negative PC
In the case of a transfusion of a RhD-positive PC to a RhD-negative women of childbearing age, 250 IU (50 μg) of anti-D immunoglobulin should be administered, a dose able to cover the transfusion of five therapeutic doses of PC in 6 weeks
ACUTE EMERGENCY : COMPATIBILITY
During an acute emergency, the blood bank may send group O (and possibly RhD negative) blood, especially if there is any risk of errors in patient identification. This may be the safest way to avoid a serious mismatched transfusion, in such situations.
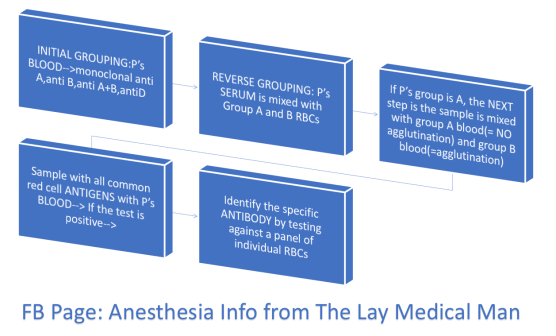
HOW A GROUP AND SAVE IS PERFORMED? (P’s = Patient’s)
#BloodTransfusion , #ABO , #BloodGroup , #TransfusionMedicine , #Anaesthesia , #Anesthesia , #Bloodbank
Reference: The Clinical Use of Blood, Handbook, WHO,
Recommendations for the transfusion of plasma and platelets Giancarlo Liumbruno, Francesco Bennardello, […], and as Italian Society of Transfusion Medicine and Immunohaematology (SIMTI) Working Party
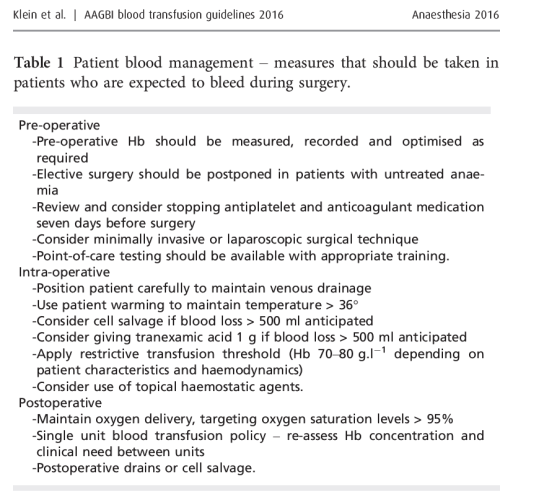
AAGBI GUIDELINES 2016
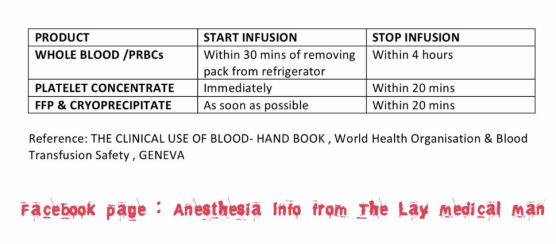
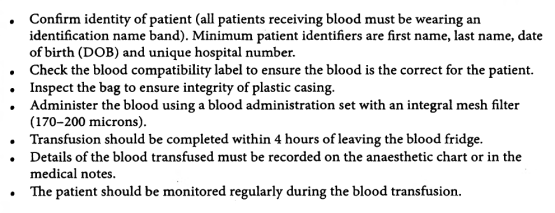
HOW WILL YOU TRANSFUSE THE BLOOD?
Also preoperatively the need for transfusion must have been explained and written informed consent should have been taken
A general Hb threshold of 7.0 g/dl should apply as a guide for red cell transfusion. 8.0 g/dl for patients with IHD
ALSO NOTE:
• A transfusion of 10 ml/kg of RBC should increase Hb by approximately 2.0 g/dl-
• Cryoprecipitate should be given in a dose of 5–10 ml.kg-1
• Platelets should be given in a dose of 10–20 ml.kg-1.
• Fresh frozen plasma may be given in doses of 10–15 ml.kg-1.
Tranexamic acid can be used in children: a loading dose of 15 mg.kg-1 followed by infusion 2 mg.kg-1.h-1 should be used in trauma