Bridging anticoagulation consists of the substitution of a long-acting anticoagulant (usually with warfarin) for a shorter-acting anticoagulant (usually LMWH) to limit the time of subtherapeutic anticoagulation levels and minimize thromboembolic risk. Despite the growing evidence about the limited to nonexistent benefits of bridging therapy, it is still being used on a case-by-case basis. Clinical scenarios that may benefit from bridging therapy are those involving patients with high thromboembolic risk. In several guidelines, the following scenarios have been proposed:
- The patient with a mechanical heart valve: Mitral valve replacement, aortic valve replacement with additional risk factors (stroke, TIA, cardioembolic event, or intracardiac thrombus), more than 2 mechanical valves.
- Patients with stroke, episode of systemic emboli, or VTE during the last 3 months. Patients presenting with a thromboembolic event after interruption of chronic anticoagulation therapy or those presenting with VTE while on therapeutic anticoagulation.
- Patients with atrial fibrillation and CHA2DS2VASc score > 5 plus additional cardiovascular risk factors (rheumatic valve disease, stroke, or systemic embolism within the last 12 weeks). A CHA2DS2VASc score > 6 with or without additional risk factors.
- Patients with recent coronary stenting (within the previous 12 weeks)
How to bridge?
During the preoperative period:
- Discontinue warfarin five days before surgery.
- Three days before surgery, start subcutaneous LMWH or unfractionated heparin (UFH), depending on the renal function of the patient at therapeutic doses.
- Two days before surgery assess INR, if greater than 1.5 vitamin K can be administered at a dose of 1 to 2 mg.
- Discontinue LMWH 24 hours before surgery or 4 to 6 hours before surgery if UFH.
During the postoperative period:
- If the patient is tolerating oral intake, and there are no unexpected surgical issues that would increase bleeding risk, restart warfarin 12 to 24 hours after surgery.
- If the patient received preoperative bridging therapy (high thromboembolic risk) and underwent a minor surgical procedure, resume LMWH or UFH 24 hours after surgery. If the patient underwent a major surgical procedure, resume LMWH or UFH 48 to 72 hours after surgery.
- Always assess the bleeding risk and adequacy of homeostasis before the resumption of LMWH or UFH
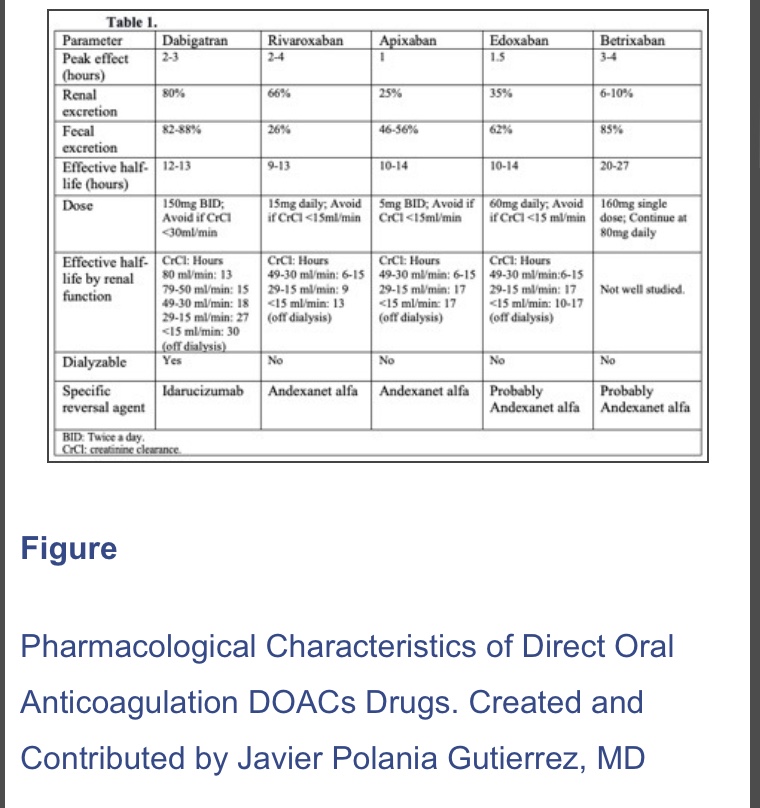
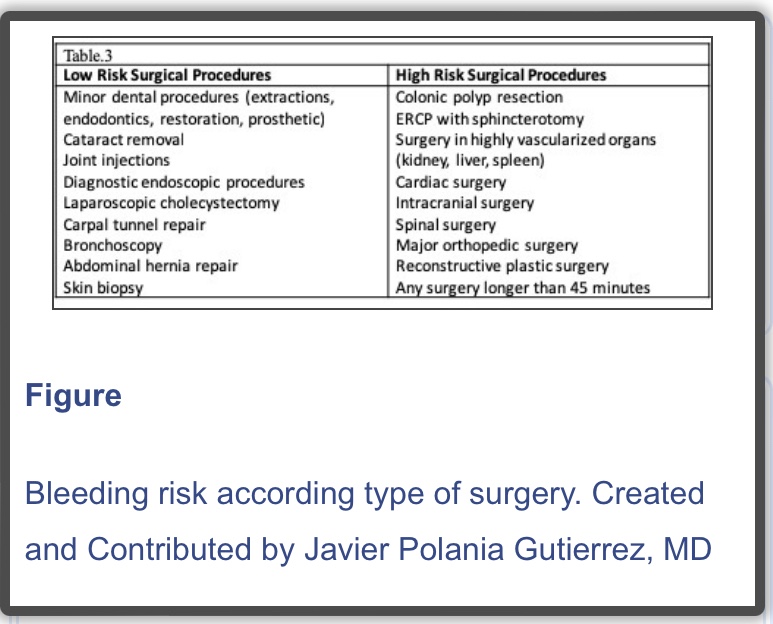
N.B. : In 2019, a new strategy was published in the PAUSE study, a prospective clinical trial evaluating a standardized approach for perioperative management of DOACs. The interruption scheme used in this study was simple. For high bleeding risk procedures, rivaroxaban, apixaban, and dabigatran were suspended 48 hours before surgery in patients with CrCl>50 ml/min. If the renal function was compromised (CrCl< 50 ml/min), these drugs were interrupted for four days before surgery. For low bleeding risk procedures, rivaroxaban, apixaban, and dabigatran were interrupted 24 hours before surgery in patients with CrCl>50 ml/min. If the renal function was compromised (CrCl <50 ml/min), drugs were suspended two days before the procedure. Regardless of renal function, all drugs were reinitiated at 48 hours for high bleeding risk surgical procedures and 24 hours for low bleeding risk procedures. The 30-day postoperative rate of major bleeding was 1.35% (95% CI, 0%-2.00%) and rate of arterial thromboembolism of 0.16% (95% CI, 0%-0.48%). However, more studies are needed in patients with high surgical bleeding risk, before implementing this in regular clinical practice
Reference:
Perioperative Anticoagulation Management – StatPearls – NCBI by Polania Gutierrez JJ, Rocuts KR. · 2021
https://www.ncbi.nlm.nih.gov/books/NBK557590/