- NIV is a technique of providing ventilation without the use of an artificial airway.
- NIV has two primary pressure settings
-
The inspiratory positive airway pressure (IPAP) is similar to the peak airway pressure in traditional mechanical ventilation. A higher IPAP level would result in a larger tidal volume and minute ventilation.
-
The expiratory positive airway pressure (EPAP) is the same as PEEP during mechanical ventilation or CPAP during spontaneous breathing. In addition to its ability to improve oxygenation by increasing the functional residual capacity, EPAP also relieves upper airway obstruction with its splinting action.
-
SpO2, Capnography, PaO2, PaCO2 etc may be used for the titration of appropriate IPAP and EPAP levels.
-
CPAP (Continuous positive airway pressure) provides positive airway pressure during spontaneous breaths and it does not include any mechanical breaths. For this reason, the work of breathing is entirely assumed by the patient. CPAP is active when IPAP=EPAP. CPAP is the treatment of choice for obstructive sleep apnea without significant carbon dioxide retention. CPAP should not be used in apnea due to neuromuscular causes, if there is progressive hypoventilation or facial trauma
-
Bilevel PAP (Bilevel positive airway pressure) provides IPAP which controls peak inspiratory pressure during inspiration and EPAP that controls end-expiratory pressure. Indications are acute respiratory failure and acute hypercapnic exacerbations of COPD
-
In patients with acute cardiogenic pulmonary edema, CPAP or bilevel PAP ventilation has been found to reduce the need for subsequent mechanical ventilation
-
Inability to protect the airway from secretions or aspiration, apnoea, facial trauma are contraindications for NPPV.
- We can use nasal or oronasal mask as the interface for delivering NIV
Category Archives: Mechanical Ventilation
WHEN VENTILATOR GIVEs ALARM & SHOWS ‘PATIENT-DEMAND IS HIGH’ : Troubleshooting the Ventilator
Check for causes:
Increased airway resistance- if so give bronchodilators
Anxiety–> increased RR + muscle tension–> increased airway resistance –> increased demand: Optimise sedation
Check for leaks in circuit and correct
If flow rate seems too low: Set higher inspiratory flow rate or reduce inspiratory time especially if patient is showing tachypnea
If Tidal volume or RR set too low: Increase it
Double triggering or breath stacking can happen if inspiratory time set is lower compared to that of the patient and ventilatory demand is high: Try increasing the inspiratory time or change to pressure control modes
NB:
Peak Inspiratory Pressure high with normal Plateau Pressure = it’s Increased airway resistance
Both (a)Peak Inspiratory Pressure and (b)Plateau Pressure are high and (a)-(b) is normal= it’s reduced compliance or auto peep
#CriticalCare , #MechanicalVentilation ,#VentilationBasics , #Ventilation , #anesthesia , #anesthesiologist , #ICUnurse , #ICUdoctor , #ICU
MECHANICAL VENTILATION FACTS
STATIC COMPLIANCE, DYNAMIC COMPLIANCE & PLATEAU PRESSURE
Compliance is a measurement of the distensibility of the lung
Compliance of both the chest wall and the lung tissue is known as Total Lung Compliance
Total Lung Compliance = Change in volume / Change in pressure
Static Compliance is the truest measure of the compliance of the lung tissue
It is measured when there are no gases flowing into or out of the lungs
Static Compliance = Exhaled Tidal Volume / (Plateau Pressure-PEEP)
The Plateau Pressure is obtained by instituiting a 2 second inspiratory pause at the peak of inspiration. This pause creates the condition of no gases flowing into the lungs.
This reflects the pressure due to the elastic recoil forces of the lung tissue alone . No pressure resulting from the flow of gases is measured.
Normal value for Static Compliance is 70-100 mL/cm H2O. This means that for every 1 cm H2O pressure change in the lungs , there is a change in volume of 70-100 mL of gas
As Dynamic Compliance is a measurement taken while gases are moving in the lungs , it measures both the Compliance of the lung tissue and the resistance to air flow
It is easier to obtain as it doesn’t require the inspiratory hold maneuver
Dynamic Compliance = Exhaled Tidal Volume / (Peak Inspiratory Pressure-PEEP)
The normal value for Dynamic Compliance is 50-80 mL/cm H2O
Dynamic Compliance measures are always smaller than Static Compliance because Peak Airway Pressure is always greater than Plateau Pressure
A decrease in Dynamic Compliance may indicate a decrease in lung compliance or an increase in airway resistance.
HUMIDIFIERS
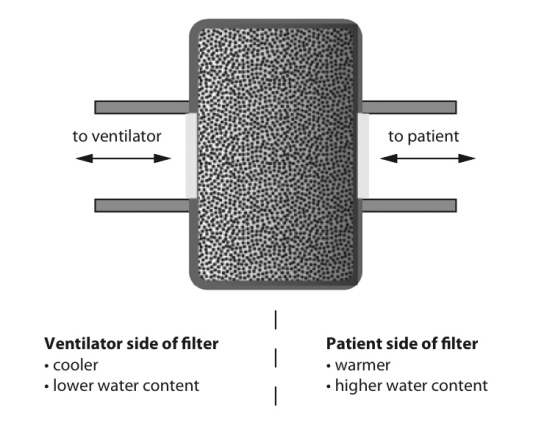
Heat and moisture exchange filter (HMEF)
- HMEF is inexpensive, disposable, passive and efficient enough to provide adequate humidification of dry gases for up to 24 hours.
- It creates a sealed unit, near the patient end of the breathing system, containing a hygroscopic material such as calcium chloride or silica gel.
- As the warm and moist gas from the patient reaches the HMEF, the moisture from the gas condenses onto the hygroscopic surface, simultaneously heating the element via the latent heat of condensation
- With the next inspiration of dry cold gas over the moist element this process is reversed, warming and humidifying the gas the patient receives.
- This process is about 80% efficient
- The addition of a 0.2 mm filter renders the interface impermeable to bacteria and viruses
- The disadvantages are that because it is a passive device, the HMEF is not 100% efficient and the patient will therefore lose heat and moisture over time, although this is negligible. Also, it adds dead space ranging from 8 mL in a paediatric HMEF to 100 mL in an adult, while the additional resistance can be up to 2.0 cm H2O ( may not create issues if respiratory function is not compromised significantly).
- The hygroscopic material and filter can act as a dam to secretions, greatly increasing the work of breathing. This is easily remedied by vigilance and replacement.
Water bath humidifiers
- Active water baths can achieve 100% efficiency and can also be used to heat the patient
- But they are bulky and complex and better suited for patients requiring longer-term ventilation or oxygen therapy.
- Passive water baths simply consist of a chamber of water through which the inspired gas is bubbled to achieve full saturation.
- The disadvantage is that the temperature of the water limits the maximum achievable humidity.
- Cooling of the water bath happens secondary to the latent heat of vaporization as the water is vaporized. This is remedied by an active system incorporating a heating element and thermostat.
- The system is designed to keep the water bath at a specific temperature (40–60°C). This increases the temperature of the gas mixture and therefore the achievable humidity. This system is capable of delivering fully saturated gas at 37°C at high flow rates which represents a significant advantage over the HMEF.
- All water baths need to include a water trap in their design, because the cooling of the gas as it moves away from the hot bath to the patient will result in condensation which can accumulate and could result in wet drowning. This risk may be minimized by heating the tubing and preventing condensation forming.
- Water baths at around 40°C minimize the risk of scalding the patient’s airways with overly heated gas, but run the risk of creating an ideal environment for microbial growth.
- By heating the water to 60°C the risk of bacterial contamination is reduced but the gas temperature must now be very carefully monitored.
- A thermistor on a feedback loop to the water bath’s thermostat can adjust the temperature of the water, and therefore inspired gas, to ensure that the patient does not suffer from airway scalding.
- The ideal size of water droplets for humidification is 5–10 microns. Smaller droplets will descend to the alveoli and larger ones will condense in the trachea.
- Scalding is a risk associated with water bath types when the temperature within exceeds 37C.
- Nebulisers are more efficient than water bath types of humidifiers. The Bernoulli effect describes the drop in pressure occurring at a jet, where velocity is greatest, which is employed to draw up water from a reservoir. This effect is used in spinning disc and gas driven humidifiers among others.
NEGATIVE PRESSURE PULMONARY OEDEMA
# NPPO is associated with upper airway obstruction in a spontaneously breathing patient.
# It occurs in 0.05–0.1% of all general anaesthetic cases and laryngospasm has been reported as being the cause in 50% of cases.
#The clinical course is most frequently observed on emergence from anaesthesia where incomplete recovery from general anaesthesia increases the likelihood of the development of laryngospasm, but it has also been reported after airway obstruction with a foreign body and blockage and biting of tracheal tubes, hanging, and strangulation.
#Pulmonary oedema is typically described as developing within 2 min of the obstruction.
Once the airway is occluded, the spontaneously breathing patient will continue to generate negative intrathoracic pressure which will increase substantially as respiratory distress develops.
#There is an associated increase in sympathetic tone due to the stress of hypoxia and airway obstruction which increases SVR and elevates pulmonary artery pressure.
This is further exacerbated by hypoxic pulmonary vasoconstriction.
#The combination of these processes creates a pressure gradient across the capillary–alveolar membrane which favours the movement of fluid into the lung parenchyma.
#It is most common in younger patients, presumably because they are able to generate higher negative inspiratory pressures and, arguably, have a higher sympathetic tone and better cardiac function.
#The condition may resolve rapidly after definitive management of the airway obstruction, but in some cases, copious pulmonary oedema may form and it can be associated with pulmonary haemorrhage suggesting capillary membrane damage.
#After recognition of the cause of obstruction, the treatment required ranges from relatively modest support such as brief periods of CPAP for 2 h to positive pressure ventilation over a period of 24 h.#TheLayMedicalMan
Ref: Neurogenic pulmonary edema, Ronan O’Leary, Justin McKinlay, Contin Educ Anaesth Crit Care Pain (2011) 11 (3): 87-92.
http://feeds.feedburner.com/TheLayMedicalMan






