Low flow anesthesia allows for economy of volatile anesthetics, makes possible heating and humidification of gases and reduces environmental pollution
Sodalime contains 94% Calcium hydroxide, 5% Sodium hydroxide and also Potassium hydroxide, Silica and dying agent
CO2 + 2NaOH –> Na2CO3 + water + heat
Na2CO3 + Ca(OH)2 –> 2NaOH + CaCO3
..this sequence gets back Sodium hydroxide
1 Kg of Sodalime can absorb >120 L of CO2
Carbon monoxide which is a byproduct of protein metabolism can accumulate in the system, but levels are <4%
If there is intoxication by alcohol or poisoning by Carbon monoxide or severe diabetic ketosis, alcohol or CO or acetone from the expired gases, will recirculate and accumulate inside the system; so low flow anesthesia is contraindicated in such states
Prolonged anesthesia with sevoflurane may generate Compound A inside the system, which can cause acute tubular necrosis in rats at concentrations around 250 ppm, a dose that is nearly 200 times seen in clinical practice. So any proteinuria, glycosuria or enzymuria which does develop in such a context has not been shown to have any clinical significance, even in patients with pre-existing renal disease
Reference: Al-Shaikh B, Stacey S. Essentials of Anaesthetic Equipment, 2nd edn. Edinburgh: Churchill Livingstone, 2002; pp. 74–9 . Nunn G. Low-flow anaesthesia. Contin Educ Anaesth Crit Care Pain 2008; 8: 1–4.


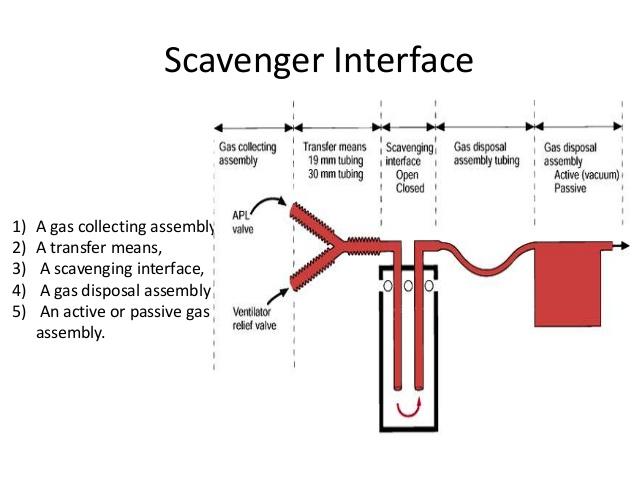 Scavenging refers to the method of extracting waste gases from the breathing system and venting them to an area where they will not be directly inhaled by staff or other patients.
Scavenging refers to the method of extracting waste gases from the breathing system and venting them to an area where they will not be directly inhaled by staff or other patients.