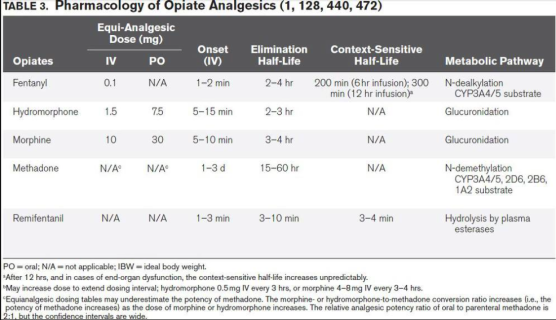
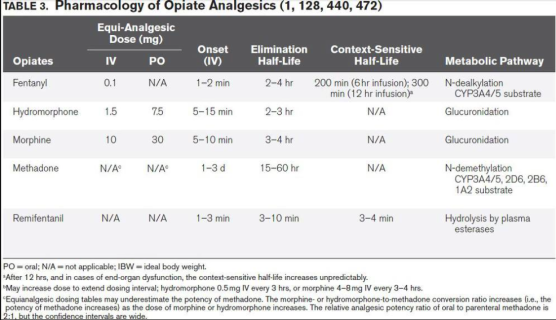
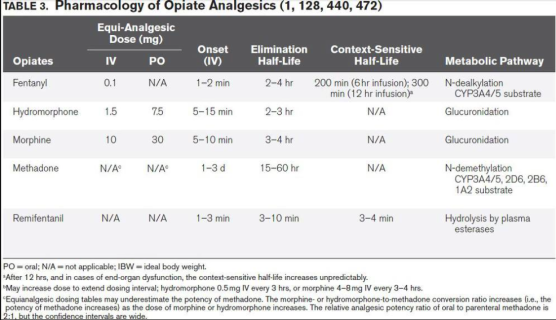
OPIOID PHARMACOLOGY

1) in a patient recovered from acute HBV: Anti HBsAg , Anti HBcAg Ig G
2) in a C/C carrier : HBsAg , Anti HBcAg Ig G
3) after immunisation : Anti HBsAg
4) best indicator of infectivity: HBeAg
5) best indicator of replication : HBV DNA
6) marker for window period : Anti HBcAg IgM
7) protective antibody : Anti HBsAg
8) acute infection : HBsAg, Anti HBcAg Ig M (plus in high virus load HBeAg and in low level infection Anti HBeAg)
![]() 💦 FFP : 15 ml/kg
💦 FFP : 15 ml/kg
![]() 💦 PC :10 ml/kg
💦 PC :10 ml/kg
![]() 💦 F VIII : % of desired rise x body weight x 0.5
💦 F VIII : % of desired rise x body weight x 0.5
TOF response %of receptors occupied
0 —————–100
1 ——————95
2—————— 90
3 ——————85
4 —————-<75
Ref: Quest to determine the ideal position of the central venous catheter tip D. K. Tempe1,* and S. Hasija, British Journal of Anaesthesia 118 (2): 148–50 (2017)
ARMITAGE : The dosage prescription scheme of Armitage :
With 0.5 mL/kg, all sacral dermatomes are blocked. •
With 1.0 mL/kg, all sacral and lumbar dermatomes are blocked. •
With 1.25 mL/kg, the upper limit of anesthesia is at least midthoracic.
However, when 1.25 mL/kg is injected there is a danger of excessive rostral spread (above T4); it is therefore preferable not to administer more than 1.0 mL/kg of local anesthetic.
EPIDURAL:
Bupivacaine, levobupivacaine- initial dose : Solution: 0.25% with 5 µg/mL (1/200,000) epinephrine
Dose:<20 kg: 0.75 mL/kg20-40 kg: 8-10 mL (or 0.1 mL/year/number of metameres)>40 kg: same as for adults
Continuous infusion- maximum doses: <4 mo: 0.2 mg/kg/hr (0.15 mL/kg/hr of a 0.125% solution or 0.3 mL/kg/hr of a 0.0625% solution)4-18 mo: 0.25 mg/kg/hr (0.2 mL/kg/hr of a 0.125% solution or 0.4 mL/kg/hr of a 0.0625% solution)>18 mo: 0.3-0.375 mg/kg/hr (0.3 mL/kg/hr of a 0.125% solution or 0.6 mL/kg/hr of a 0.0625% solution
Ropivacaine : initial dose: Ropivacaine : 0.2% Dose: same regimen in mL/kg as for bupivacaine (see above)
Infusion : Same age-related infusion rates in mg/kg/hr as for bupivacaine (usual concentration of ropivacaine: 0.1%, 0.15%, or 0.2%)Do not infuse for more than 36 hr in infants < 3 ms
DOSING ACCORDING TO SEGMENT :
The volume of local anesthetic necessary for analgesia/anesthesia depends on location of surgery and epidural catheter. In young children the estimated volume would be: 0.04 mL/kg/segment. In children older than 10 years of age simple formula can be used: V (in mL) = 1/10 x (age in years).
TEST DOSE: The recommended test dose is 0.1mL/kg of local anesthetic with 5mcg/mL of epinephrine to maximum volume of 3mL (or 2.5 mcg/mL in the child less than 18 month old )
MNEMO> First 4 letters of ACHAsia.
A. Acute upper airway obstruction secondary to tracheal compression (by the dilated segment ) can be managed by Sublingual glyceryl nitrate,Passage of a naso-oesophageal tube,Transcutaneous needle puncture,Tracheal intubation etc
C Care against aspiration: The dilated oesophagus must be emptied and decompressed (needs a period of prolonged starvation) Rapid sequence induction ,Tracheal tube removal is performed in the awake patient, Patient should be nursed in the lateral position during recovery.
H History: Respiratory complications, which may be attributed to asthma or chronic bronchitis, are secondary to overspill of undigested material
A Acute problems that can be caused by the dilated segment : Acute thoracic inlet obstruction , difficulty in passing the tracheal tube past the dilated oesophagus, Upper airway obstruction , progressive dilatation of the upper oesophagus may occur in association with air swallowing or IPPV
Remember the acronym SOAPME.
![]() 🔘S (suction) – Appropriate size suction catheters and functioning suction apparatus.
🔘S (suction) – Appropriate size suction catheters and functioning suction apparatus.
![]() 🔘O (oxygen) – Reliable oxygen sources with a functioning flow meter. At least one spare E-type oxygen cylinder.
🔘O (oxygen) – Reliable oxygen sources with a functioning flow meter. At least one spare E-type oxygen cylinder.
![]() 🔘A (airway) – Size appropriate airway equipment: • Face mask • Nasopharyngeal and oropharyngeal airways • Laryngoscope blades • ETT • Stylets • Bag-valve-mask or equivalent device.
🔘A (airway) – Size appropriate airway equipment: • Face mask • Nasopharyngeal and oropharyngeal airways • Laryngoscope blades • ETT • Stylets • Bag-valve-mask or equivalent device.
![]() 🔘P (pharmacy) – Basic drugs needed for life support during emergency: • Epinephrine (adrenaline) • Atropine • Glucose • Naloxone (reversal agent for opioid drugs) • Flumazenil (reversal agent for benzodiazepines).
🔘P (pharmacy) – Basic drugs needed for life support during emergency: • Epinephrine (adrenaline) • Atropine • Glucose • Naloxone (reversal agent for opioid drugs) • Flumazenil (reversal agent for benzodiazepines).
![]() 🔘M (monitors): • Pulse oximeter • NIBP • End-tidal CO2 (capnography) • Temperature • ECG
🔘M (monitors): • Pulse oximeter • NIBP • End-tidal CO2 (capnography) • Temperature • ECG
![]() 🔘E (equipment): • Defibrillator with paddles • Gas scavenging • Safe electrical outlets (earthed) • Adequate lighting (torch with battery backup) • Means of reliable communication to main theatre site
🔘E (equipment): • Defibrillator with paddles • Gas scavenging • Safe electrical outlets (earthed) • Adequate lighting (torch with battery backup) • Means of reliable communication to main theatre site
#anaesthesia , #anesthesiacheck , #anesthesiatechnician ,#na , #nurseanaesthetist , #nurseanesthetist , #OperatingRoomSafety , #OR , #OperationTheatre , #AnaesthesiaTechnician ,#OT ,#nora ,#aoor
NB:
MITRAL VALVE-AREA
Normal valve surface area 4 – 6 cm2
Symptom free until 1.5 – 2.5 cm2
Moderate stenosis 1 – 1.5 cm2
Critical stenosis <1 cm2