CVS:
- Average HR is 120-180 bpm and SBP 50-90 mm of Hg at birth
- Oxygen consumption is twice that of an adult 7 ml/kg/min. But because of a fixed stroke volume, increasing the HR is the only way to increase CO. Also neonatal myocardium consists of more non-contractile connective tissue.
- Parasympathetic system is predominant; bradycardia can happen in response to hypoxia or tracheal suction. Asystole is the most common form of cardiac arrest and ventricular fibrillation is uncommon
- Circulating volume approx 90 ml/kg @ birth (300-400 ml in an average neonate). Bleeding contributes proportionately a greater loss of total volume in a neonate, compared to an adult. Right ventricular mass equal to left ventricular mass until 6 months of age, resulting in right axis deviation on the ECG.
- Transitional circulation: Before birth the SVR is low due to the low resistance placental circulation whereas the pulmonary resistance is high. At birth the SVR rapidly increases after clamping of the umbilical cord and PVR decreases following functional closure of foramen ovale (due to increased venous return to left atrium from pulmonary arteries) and ductus arteriosus (in response to increased PaO2 in blood). But this can be reversed back to the foetal state due to stimuli including hypoxia, heypecarbia and acidosis, leading to a perpetuating cycle of worsening hypoxia. This is known as transitional circulation or prsistent foetal circulation.
AIRWAY/ RESPIRATORY SYSTEM
- Relatively larger head, short neck, large tongue and narrow nasal passages.
- High anterior larynx (level C2/3 compared to C5/6 in the adult).
- Large U-shaped floppy epiglottis.
- Narrowest point of the larynx is at the level of the cricoid cartilage (in adults it is at the laryngeal inlet).
- Trauma to the small airway can easily lead to oedema and airway obstruction. 1 mm oedema can narrow an infant’s airway by 60% (resistance ∝1/radius).
- Equal angles of mainstem bronchi (in adults the right main bronchus is more vertical).
- A compliant chestwall: FRC is less as the elastic recoil pulls the compliant chest wall inwards. Closing volume is larger than FRC until 6–8 years of age resulting in airway closure at end-expiration; this can be reduced by CPAP
- Fatiguable respiratory and accessory muscles: The diaphragm has less % of fatigue resistant type I respiratory fibres. Raised abdominal pressure can splint the diaphragm precipitating respiratory failure. Diaphragmatic breathing > intercostal breathing. Diaphragmatic movement restricted by relatively large liver.
- Horizontally aligned ribs prevent the bucket handle movement of the ribs during inspiration
- Incompletely developed alveoli.Born with only 10% of the total number of alveoli as adults. Alveoli develop over first 8 years. Higher alveolar ventilation 100–150 mL/kg/min compared with 60 mL/kg/min in adult.
- Inconsistant ventilatory response to hypercapnoea. Higher risk of apnoea
- Sinusoidal respiratory pattern, no end-expiratory pause (inspiratory/expiratory ratio 1:1). Resting repiratory rate is high and increases further if respiratory compensation is required. Limited capability to increase the tidal volume
- Obligate nasal breathers; nasal obstruction (e.g. choanal atresia, respiratory infection) can precipitate respiratory failure
- MAC infant > neonate > adult
CNS
- CNS development is incomplete at birth
- Myelination starts before birth and continues throughout the first year
- Spinal cord ends at L3 (L1 by age 2 years).
- Unfused fontanelle and sutures makes it more compliant and can expand to some extent in response to raised ICP. ICP is less than the adult: 2-4 mm of Hg
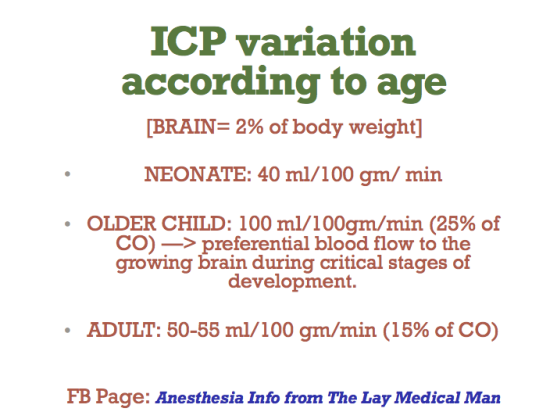
- Cerebral Blood Flow is less in the neonate than the adult and autoregulation operates at less SBPs
- In premature infants autoregulation is absent and perfusion is pressure dependent
- Blood brain barrier is more permeable and hence the neonate is more sensitive to sedatives
- Neonate responds to pain with tachycardia, hypertension, grimaces etc
TEMPERATURE REGULATION
-
Higher thermoneutral temperature (temperature below which an individual is unable to maintain core body temperature) 32 degree C for a term infant compared with 28 for an adult.
- Neonate loss heat very readily due to a high body surface area to weight ratio and absence of shivering in infants ❤ months
- Produces heat by metabolism of brown fat (5-6% of body wt, stored around kidneys, scapula and mediastenum) by non shivering thermogenesis. Beta adrenergic mediated and contributes to significant amount of the O2 demand placed on the cardiorespiratory system. Ablated by beta blockade
RENAL SYSTEM
- Immature at birth
- Higher total body water (80%) at birth
- Renal blood flow is 6% of cardiac output at birth rising to 18% of cardiac output at 1 month (compared with 20% in adult).
- Reduced GFR, tubular function until 6–8 months of age
- Reduced H+ ion excretion
- Cannot tolerate both excessive water/ sodium load and dehydration (decresed ability to conserve water)
- Fluids must be carefully balanced based on weight, insensible and observed fluid losses and maintenance requirements
HEPATIC SYSTEM
Low hepatic glycogen stores means hypoglycaemia occurs readily with prolonged fasting
DRUG ADMINISTRATION
- TBW is increased: so the volume of distribution of water soluble drugs will increase and hence need an increase in the dose. e.g. Succinyl choline (1 mg/kg in adult but 2 mg/kg in the neonate)
- Succinyl choline by acting on the SA node can produce arrhythmias and even asystole in the neonate
- Though the neonate is more sensitive to nondepolarizing muscle relaxants, the higher ECF volume increases the required dose; so the final required dose remains unchanged
- Immature hepatic and renal systems make the metabolism and excretion of the drugs slow. e.g. half life of morphine is increased due to the reduced ability to produce glucoronide conjugates
- Circulating levels of albumin and alpha acid glycoprotein is less, increasing the free fraction and a pronounced effect
-
MAC is age related. MAC values for an infant are: • sevoflurane = 3.3% • isoflurane = 1.9% • desflurane = 9.4%.
