- From a practical standpoint, requirement for > 4 RBC units in 1 hour with ongoing need for transfusion, or blood loss > 150 ml/min with hemodynamic instability and need for transfusion are reasonable definitions in the setting of a massive transfusion situation. Other definitions are >loss of more than one blood volume within 24 hours (around 70 mL/kg, >5 litres in a 70 kg adult), 50% of total blood volume lost in less than 3 hours or bleeding in excess of 150 mL/minute. A pragmatic clinically based definition is bleeding which leads to a systolic blood pressure of less than 90 mm Hg or a heart rate of more than 110 beats per minute.
- Hypoperfusion leads to lactic acidosis, systemic inflammatory response syndrome (SIRS), disseminated intravascular coagulation and multiorgan dysfunction
- Hypoperfusion, acidosis, hemodilution due to iv fluids and progressive hypothermia influences the pathophysiology of massive transfusion in a big way
- Hypothermia and acidosis play a key role by reducing thrombin generation due to altered enzyme kinetics. After 2 weeks of storage, PRBCs have a pH below 7.0, and each unit has an acid load of approximately 6 mEq. Acidosis directly reduces activity of both extrinsic and intrinsic coagulation pathways. A pH decrease from 7.4 to 7.0 reduces the activity of FVIIa and FVIIa/TF by over 90% and 60% respectively. Both coagulation factors and platelets are reduced by hemodilution. NB: High ISS scores, shock, high base deficit and increased INR > 1.5 are associated with increased mortality in the pediatric population
- Collect blood sample for cross match early as colloids may interfere with cross matching (mainly dextrans by coating RBC surface)
- Red cell transfusion is usually necessary if 30–40% blood volume is lost, and rapid loss of >40% is immediately life threatening. Peripheral blood haematocrit and Hb concentration may be misleading early after major acute blood loss. False values occur with TEG too in certain situations. Higher hemoglobin levels reduce TEG/ROTEM signals. Conversely, low hemoglobin makes signals larger.
- ABO-group-specific red cells can usually be issued within 10 minutes of a sample arriving in the laboratory. Fully crossmatched blood is available in 30 to 40 minutes after a sample is received in the laboratory. For immediate transfusion, group O red cells should be issued after samples are taken for blood grouping and crossmatching. Females less than 50 years of age should receive RhD negative red cells to avoid sensitisation.
- Once the volume of blood transfused in any 24 hour period is equivalent to the patient’s own blood volume (8–10 units for adults and 80–100 mL/kg in children), ABO and D compatible blood can be issued without the need for a serological crossmatch.
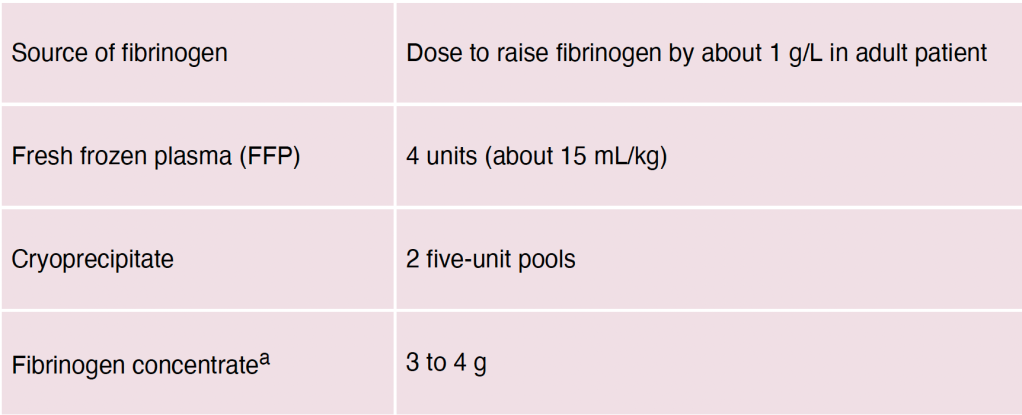
- Fibrinogen Level: Plasma fibrinogen predictably falls to sub-haemostatic levels (<1.5 g/L) after 1 to 1.5 blood volume replacement (earlier in the presence of coagulopathy and hyperfibrinolysis). A threshold level of fibrinogen 1g/L (100 mg/dL) is reached after losing 150% of circulating blood volume as opposed to 200% for clotting enzymes. A fibrinogen level lower than < 1g/L substantially increases in-hospital mortality.
- Coagulation is also impaired by reduced ionised calcium (Ca2+) concentration (which can be measured on many blood gas analysers). Ionised hypocalcaemia may be caused by rapid transfusion of blood components containing citrate anticoagulant, although this is uncommon in the presence of normal liver function
- The fibrinolytic pathway is relatively preserved despite hemodilution. Fibrinolysis is actually increased due to dilution of FXIII and α2 –antiplasmin which reduces fibrin cross-linking, decreases resistance to fibrinolysis and prolongs plasmin half-life. Plasminogen activator inhibitor is decreased, prolonging tissue plasminogen activator (tPA) activity. Stress, thrombin, epinephrine, vasopressin, desmopressin, and bradykinin trigger tPA release. CRASH-2, MATTERs and PED-TRAX studies suggested a survival advantage with administration of Tranexamic Acid.
- FFP should be transfused in doses of 12–15 mL/kg (at least four units in the average adult) to maintain the PT ratio (compared to ‘normal pooled plasma’) less than 1.5. Fibrinogen levels should be maintained above 1.5 g/L
- Large-volume FFP transfusion carries increased risks of circulatory overload (TACO), allergic reactions and transfusion-related acute lung injury (TRALI)
- The platelet count usually remains above 50000/uL (the generally accepted haemostatic level) until 1.5 to 2.5 blood volumes have been replaced. An adult therapeutic dose should be requested when the count falls to 75000-100000/uL.
- Systematic reviews and registry studies show no good evidence of improved survival with the use of recombinant activated factor VIIa and life-threatening arterial and venous thromboembolic complications may occur
- Point‑of‑care testing is highly desirable: Arterial blood gas (ABG) and thromboelastograph (TEG). ABG with haemoglobin (Hb), electrolyte and lactate levels, repeated hourly, are useful in directing therapy
- A few words about citrate toxicity: 80 ml of citrate phosphate dextrose adenine solution present in each blood bag contains approximately 3 g citrate. A healthy adult can metabolise this load in 5 min. However, hypoperfusion or hypothermia associated with massive blood loss can decrease this rate of metabolism leading to citrate toxicity. Unmetabolised citrate can then lead to hypocalcaemia, hypomagnesemia and worsen the acidosis. Hypocalcaemia can lead to myocardial depression that manifests earlier than hypocalcaemic coagulopathy. Hypotension not responding to fluids should alert the physician to this complication. Calcium supplementation is thus required in most cases of massive transfusion
- Massive transfusion protocols (MTP) are generally activated after transfusion of 4-10 units. MTPs have a predefined ratio of RBCs, FFP/cryoprecipitate and platelets units (random donor platelets) in each pack (e.g. 1:1:1 or 2:1:1 ratio) for transfusion. The trigger for initiating the protocol as well as the optimum ratio of RBC: FFP: Platelets is controversial. Therefore practice varies from centre to centre. If MTP is triggered for a nonmassive blood loss situation, it may lead to wastage of blood products.
- Targets of resuscitation in massive blood loss: Mean arterial pressure (MAP) around 60 mmHg, systolic arterial pressure 80-100 mmHg (in hypertensive patients one may need to target higher MAP), Hb 7-9 g/dl, INR <1.5; activated PTT <42 s, Fibrinogen >1.5-2 g/L, Platelets >50000/uL, pH 7.35-7.45, Core temperature >35.0°C, Base deficit <3.0/lactates <2 mEq/L.
