- ASSESSMENT OF NEUROMUSCULAR FUNCTION
- CLINICAL:
- Grip strength
- Ability to sustain head lift for at least 5 seconds
- Ability to produce vital capacity of at least 10 mL/kg
- NEUROMUSCULAR STIMULATION EQUIPMENTS:
- Peripheral nerve stimulator
- Mechanomyography: uses force transducer to quantitatively measure contractile response
- Acceleromyography: measures movement of joints caused by muscle movement
- Electromyography: measures electrical activity associated with action potential propagation in a muscle cell (research use)
- BENEFITS
- Monitoring helps to assess the degree of relaxation, help adjust dosage, assess development of phase II block, provide early recognition of patients with abnormal cholinesterases, and to assess cause of apnoea.
- All twitches that we deliver in theatre with the nerve stimulators are uniform
and so we only need to learn a couple of facts.
• All twitches are delivered at 50 mA (i.e. supramaximal stimulus)
• All twitches last 0.2 ms
Once we have these facts, the rest becomes easier to remember - TYPES
- Single twitch is insensitive since >75% of postsynaptic receptors must be blocked before there is any diminution in twitch height. We will not see ‘fade’ during single-twitch stimulation. >> Twitch current 50 mA. Duration of twitch 0.2 ms. Frequency of twitches 1 Hz (i.e. 1 every second). Number of twitches: as many as operator chooses to give. Single twitch can be used to assess block in depolarising nmbd, i.e.
suxamethonium, where fade and post-tetanic facilitation do not occur - Train of four: >>Twitch current 50 mA. Duration of twitch 0.2 ms. Frequency of twitches 2 Hz (i.e. 2 every second). Number of twitches: 4. Compare last (T4) and first twitch (T1). TO4 ratio (T4 :T1) indicates degree of neuromuscular blockade:
- – T 4 disappears at 75% depression of T 1 (1st, 2nd and 3rd twitches present)
- – T 3 disappears at 80% depression of T 1 (1st and 2nd twitches present)
- – T 2 disappears at 90% depression of T 1 (1st twitch only)
- – T 1 disappears at 100% depression of T 1 (no twitches).
- A TO4 count of 0–1 is needed for adequate intubating conditions, but a count of three twitches provides adequate relaxation for most surgery (To4 ratio of 0.15 – 0.25) To4 ratio of > 0.9: essential for safe extubation and recovery post surgery
- A TO4 ratio >0.70, corresponds to adequate clinical recovery, but normal pharyngeal function requires a ratio >0.90.
- Neuromuscular reversal can be given when T2 has reappeared, i.e. when T1 is about 20% of its control height.
- The diaphragm is the most resistant (but with shorter onset times) of all muscles to both depolarising and non-depolarising relaxants requiring 1.5 to 2 times as much drug as the adductor pollicis muscle for an identical degree of blockade.
- A supramaximal stimulus should be truly maximal throughout the test period to maintain accuracy; hence the electrical current applied is at least 20% to 25% above that necessary for a maximal response.
- Tetanic stimulation: >> Twitch current 50 mA. Duration of twitch 0.2 ms. Frequency of twitches 50 Hz (i.e. 50 every second). Number of twitches: stimulation lasts 5 seconds = 5 × 50 = 250 twitches. With non-depolarizing block, peak height is reduced and fades. Release of acetylcholine is reduced (possibly presynaptic effect) and postsynaptic receptors are blocked, limiting sustained contraction. Tetanic stimulation is extremely painful in an awake patient and may leave an unpleasant sensation in those who were anaesthetised.
- Post-tetanic count: >> Twitch current 50 mA. Duration of twitch 0.2 ms. Frequency of twitches 1 Hz (i.e. 1 every second). Number of twitches: as many as operator chooses to give. May result in response (post-tetanic potentiation), even if none is seen with original TO4. Due to increased synthesis and mobilization of acetylcholine following tetanus. Appearance of post-tetanic count precedes return of TO4 by 30–40 min.PTC < 5 = profound block. PTC >15 = equivalent to two twitches on To4
- Double-burst stimulation: >> Twitch current 50 mA. Duration of twitch 0.2 ms. Frequency of twitches 50 Hz (i.e. 50 every second). Number of twitches: 3 twitches – break of 750 ms – 3 more twitches. Similar to TO4, but tactile evaluation is more sensitive because fade of the two resultant contractions is more marked.
- Nondepolarising neuromuscular blocking agents (NDMB): repetitive stimulation (ToF or tetanus) is associated with fade (reduction in amplitude of evoked responses with T4 affected first, then T3, followed by T2, then finally T1) and post-tetanic facilitation.
- Depolarising neuromuscular blocking agents (DMB): no fade or posttetanic facilitation observed. Repeated dose of suxamethonium can give characteristics of NDMB—phase II block).
- A PNS is Portable, battery-powered, and easy to use Able to deliver different impulses. Supramaximal current output of 50–60 mA at all frequencies can be given to ensure all nerve fibres are depolarised. Has a Monophasic square waveform. Can give Single twitch at 0.1 Hz, Train of four (TOF) at 2 Hz and Tetanic stimulation at 50 Hz
- Fade: A gradual diminution of evoked response during prolonged or repeated nerve stimulation, is indicative of a nondepolarizing block. Adequate clinical recovery correlates well with the absence of fade.
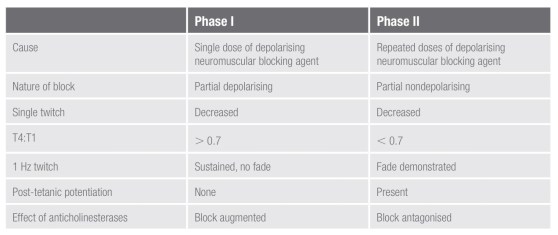
- PHASE I and PHASE II Blocks: These terms refer to the blocks seen following the administration of suxamethonium. A phase I block describes the block seen following the administration of a single dose of suxamethonium. Suxamethonium binds to the ACh receptor, which causes opening of the sodium channel and membrane depolarisation. This results in disorganised muscle contraction, seen as fasciculation followed by flaccid paralysis because suxamethonium causes prolonged depolarisation of the motor end plate. The characteristics of a phase I block:
• Reduced twitch height, but sustained response to tetanic stimulation
• No post-tetanic facilitation; does not exhibit fade during tetanus or train-of-four
• TOF ratio >70% (height of fourth twitch to that of first). This is a measure of the pre-synaptic effect of suxamethonium.
The block is potentiated by the effect of anticholinesterases because these
will further decrease the rate of suxamethonium breakdown.
A phase II block describes the block seen following the repeated administration/infusion of suxamethonium and can develop with doses
in excess of 2.5 mg/kg. It occurs because in the continued presence
of suxamethonium, the receptors eventually close and the membrane
repolarises, at least partially. However, it is now desensitised to ACh and so
cannot open again to propagate an action potentials. In this way, a phase II
block is similar to a non-depolarising block. Phase ii blocks are also called
‘desensitisation blocks’.
characteristics of a phase ii block:
• Exhibits fade on tetanic stimulation
• Exhibits post-tetanic facilitation
• TOF ratio < 0.3 (fourth to first twitch height)
• Antagonised by anticholinesterases
• Tachyphylaxis is seen with the need to increase suxamethonium infusion
rate or bolus dose.

- Post-tetanic potentiation: Tetanic stimulation is a supra-maximal stimulation, applied to the NMJ for a prolonged period of time. It is sufficient to produce a substantial increase in ACh release, enough to overcome competition from NMBA in all but the most profound of blocks. The positive feedback mechanism via prejunctional receptors by stimulating an increase in ACh production by second messenger systems gets activated and this increases the amount of ACh available for release. This is called post-tetanic potentiation.
- Commonly monitored nerves in theatre are:
• Facial nerve – twitch of the eyebrow with orbicularis oculi contraction
• Ulnar nerve – twitch of the thumb with adductor pollicis contraction
• Posterior tibial nerve – twitch of the big toe with flexor hallucis brevis contraction - Which muscles are affected first by NMBAs?
NMBAs cause paralysis of all voluntary muscles in the body, but some are
more sensitive than others. in order of decreasing sensitivity:
• Eyes (affected first)
• Facial muscles
• Neck
• Extremities
• Limbs
• Abdominal muscles
• Glottis
• Intercostal muscles (affected last).
Muscle function returns in the reverse order. This is why it is traditional to
wait until a patient can lift their head of the pillow before extubation
