- The need for cardiac pacing results from conduction disorders of the heart, which may or may not be associated with IHD.
- Permanent Pacemakers (PPM) are classified using a five letter code( See below)
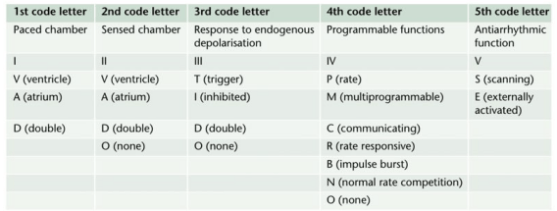
- For example DDDR means atrial and ventricular pacing (I), atrial and ventricular sensing(II) with double/adaptive (III) rate response(IV)
- Most modern units work in DDD mode, and provide atrial pacing in the presence of atrial bradycardia and ventricular pacing after an endogenous/paced atrial depolarization, if a spontaneous ventricular beat is absent
- KEY PERIOPERATIVE QUESTIONS: 1. Indication for pacemaker and associated cardiac comorbidities 2. Type of pacemaker; also how does the rate modulation work in that pacemaker? Chest x-ray will help to find the pulse generator siting and lead placement (atrium/ventricle/both) and number 3. When it was last checked 4. Requirement of diathermy for the procedure 5.Whether anticipating any other factor/s interfering with pacemaker function? 6. Surgical site proximity to the pacemaker 7. What is your plan to avoid inappropriate pacemaker function (e.g. change from demand to fixed rate mode) in case of interference? Cardiology/ Pacemaker programmer support may be needed for the same
- WHAT ECG CAN TELL: 1. If native rhythm predominates–> patient not PPM dependent 2. If all beats preceeded by a pacemaker spike–> pacemaker dependent 3. No evidence of pacemaker activity–> magnet might be applied over the pulse generator to switch to fixed rate pacing. If pacemaker is activated by a magnet to pace at a fixed rate, spike may fall in the refractory period and fail to stimulate the ventricle 4. If pacemaker spike is not followed by p or QRS waves –> PPM malfunction
- The characteristics of a PPM can be changed externally by application of a magnet or using radiofrequency generators, usually for a change of demand to fixed rate. Application of a magnet over a non-programmable VVI pacemaker will convert it to VVO asynchronous mode. The modern reprogrammable units need a cautious approach to the use of magnets. In this case, there is a risk of reprogramming ( with inappropriate settings), but it will remain in the asynchronous fixed rate mode, until the magnet is removed, after which the ‘inappropriate’ reprogrammed mode may take over
- ABOUT THE RATE RESPONSE FUNCTION: Such PPMs may sense electrical activity or vibration (e.g. shivering) and cause a tachycardia in response. Some measure respiratory rate by sensing thoracic impedence and adjust HR accordingly. Some sense blood temperature and so may cause a tachycardia when warming a hypothermic patient. With hypokalemia, there is a risk of loss of pacing capture and with hyperkalemia, there is risk of VT or VF.
- INTRAOPERATIVE STEPS: 1. If possible, avoid surgical diathermy; but if unavoidable, bipolar is safer than unipolar diathermy. 2. Monopolar where necessary, should be used in short bursts with at as low energy levels as possible 3. Diathermy plate should be kept on the same side, as far away from the PPM as possible 4. Cables from diathermy equipment also should be kept away from the PPM 5. Confirm device functionality on completion of the surgery
- Surgical diathermy can cause 1. Ventricular fibrillation 2. ‘Reprogramming’ of programmable PPMs 3. Inhibition of demand function 4. Unit failure 5. Asystole
- AUTOMATIC IMPLANTABLE CARDIOVERTER DEFIBRILLATORS (AICDs) AND THE ANESTHESIOLOGIST: They consist of a set of lead electrode systems for sensing-pacing-delivery of shocks for cardioversion/ defibrillation; modern units can also function as DDD pacemakers. In general, AICDs better be deactivated with a programming device before surgery to avoid inappropriate shock delivery due to electrical interference; in modern AICDs, the anti-bradycardia function can be left activated (Consult the manufacturer for this). The effect of magnets are inconsistent across devices; but modern units are inhibited by magnets. If required, external pads can be placed over the patient with external defibrillators ready to attach, for use in case any tachyarrhythmias occur during this period. Take all precautions as in the case of PPM. Postoperatively, the ICD should be checked and reactivated.
Category Archives: Comorbid illness and anesthesia
Management options in hypercalcemia
- Administration of normal saline
- Loop diuretics like Frusemide ( Thiazides will increase the tubular absorption of calcium)
- Calcitonin
- Bisphosphonates
- Mithramycin
- Hydrocortisone
- Hemodialysis
- Hypercalcemia per se doesn’t contraindicate any specific anesthetic drug or technique

TRANSFORMATION OF A PREGNANT LADY❗️ (When does the physiological changes of pregnancy comes back to normal?)
↪️Despite decreased requirements during pregnancy ,spinal anesthesia requirements return to non pregnant levels by 12-36 hours postpartum. Abouleish et al found that patients required 30% more bupivacaine, to achieve a T4 level for post partum tubal ligation , upto 24 hours after delivery. Rapid decline in plasma progesterone levels, after delivery of placenta is one factor, which contributes to this.
↪️Cardiac output rises immediately after delivery because of autotransfusion of 500 to 750 ml of blood from the uterus. Patients with pulmonary hypertension and stenotic valvular lesions are at a particular risk at this time.
↪️Cardiac output returns to slightly above prepregnancy values about 2 to 4 weeks after delivery.
↪️FRC and residual volume rapidly return to normal.
↪️Many of the pulmonary changes caused by mechanical compression by the gravid uterus resolve quickly. Alveolar ventilation returns to baseline by 4 weeks postpartum, and there is a rise in maternal PCO 2 as the progesterone levels decrease.
↪️The dilutional anemia of pregnancy resolves, and the hematocrit returns to normal within 4 weeks secondary to a postpartum diuresis.
↪️Serum creatinine, glomerular filtration rate, and BUN return to normal levels in less than 3 weeks.
↪️Mechanical effects of the gravid uterus on the gastrointestinal system resolve about 2 to 3 days after delivery; however, gastric emptying may be delayed for several weeks as serum progesterone levels slowly decrease.
#TubalLigation ,#pps , #PostpartumSterilization , #ObstetricAnesthesia , #ObstetricAnaesthesia, #PregnancyPhysiology ,#anesthesia , #anaesthesia ,#obstetrics , #pregnancy , #sterilization
Reference:
Shnider and Levinson's anesthesia for obstetrics, Maya Suresh; Sol M Shnider; Gershon Levinson, 2013,English : 5th
Ana M. Lobo, Andrea J. Fuller,Marina Shindell, Chapter 59, Anesthesia Secrets, 4/e
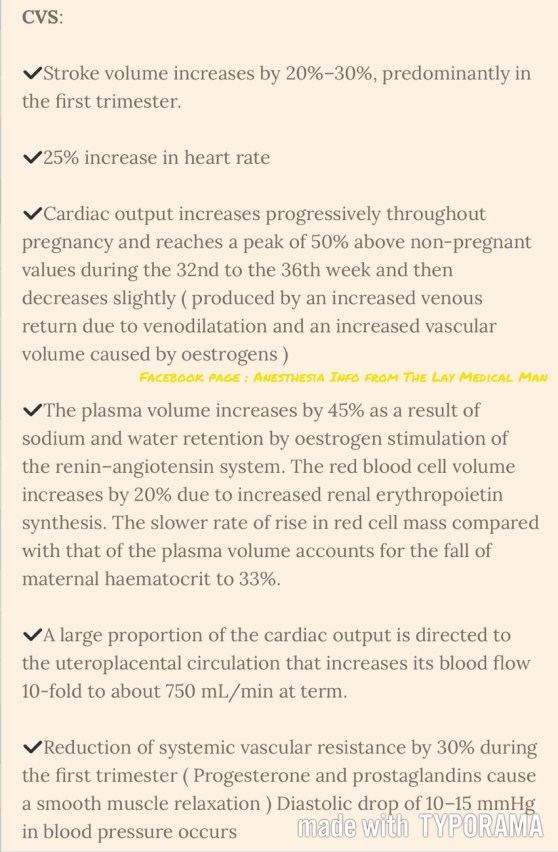
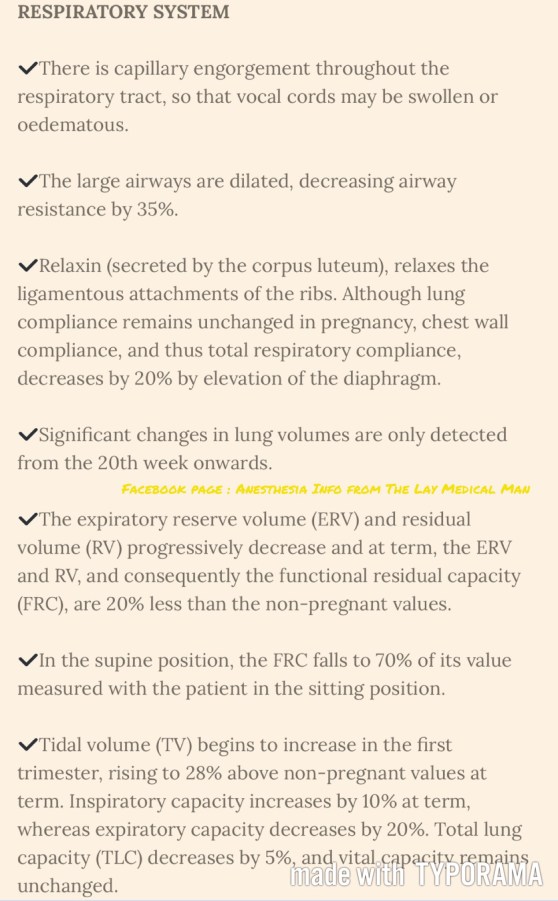
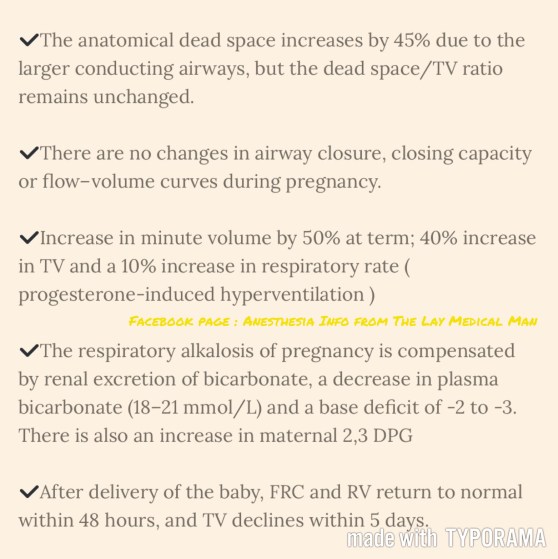
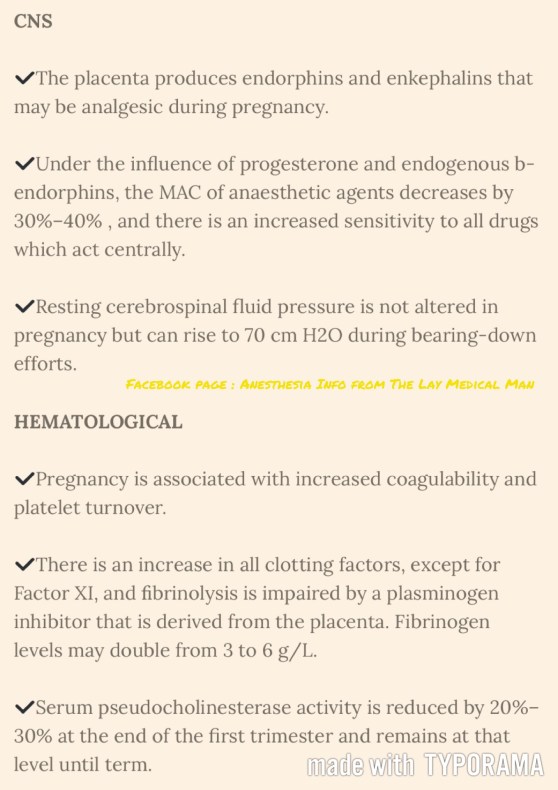
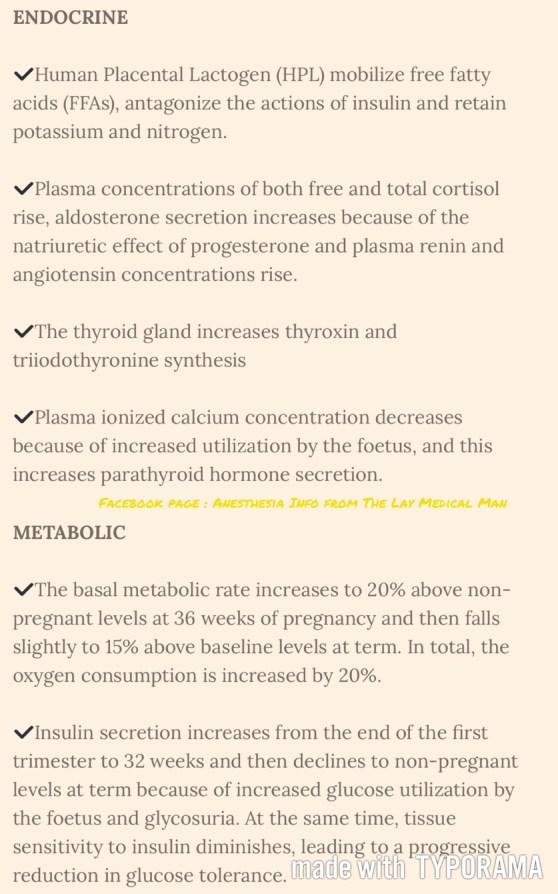
PREGNANCY: SUMMARY OF PHYSIOLOGICAL CHANGES



RESPIRATORY PHYSIOLOGY IN THE ELDERLY 👴🏻
🍃Ventilatory responses to hypoxia and hypercapnia are impaired secondary to reduced central nervous system activity.
🍃The respiratory depressant effects of benzodiazepines, opioids, and volatile anesthetics are exaggerated.
🍃These changes compromise the usual protective responses against hypoxemia after anesthesia and surgery in elderly patients.
🍃The loss of elastic recoil combined with altered surfactant production leads to an increase in lung compliance.
🍃Increased compliance leads to limited maximal expiratory flow and a decreased ventilatory response to exercise.
🍃Loss of elastic elements within the lung is associated with enlargement of the respiratory bronchioles and alveolar ducts, and a tendency for early collapse of the small airways on exhalation.
🍃There also is a progressive loss of alveolar surface area secondary to increases in size of the interalveolar pores of Kohn. This results in increased anatomic dead space, decreased diffusing capacity, and increased closing capacity all leading to impaired gas exchange.
🍃Loss of height and calcification of the vertebral column and rib cage lead to a typical barrel chest appearance with diaphragmatic flattening.
🍃The flattened diaphragm is mechanically less efficient, and function is impaired further by a significant loss of muscle mass associated with aging. Functionally, the chest wall becomes less compliant, and work of breathing is increased.
🍃Total lung capacity is relatively unchanged.
🍃Residual volume increases by 5% to 10% per decade.
🍃Vital capacity decreases.
🍃Closing capacity increases with age.
🍃Functional residual capacity (FRC) is determined by the balance between the inward recoil of the lungs and the outward recoil of the chest wall. FRC increases by 1%–3% per decade because at relaxed end expiration, the rate of decrease in lung recoil with aging exceeds that of the rate of increase in chest wall stiffness.
🍃In younger individuals, closing capacity is below functional residual capacity. At 44 years of age, closing capacity equals functional residual capacity in the supine position, and at 66 years of age, closing capacity equals functional residual capacity in the upright position.
🍃When closing capacity encroaches on tidal breathing, ventilation-perfusion mismatch occurs.
🍃When functional residual capacity is below closing capacity, shunt increases, and arterial oxygenation decreases. This results in impairment of preoxygenation. Increased closing capacity in concert with depletion of muscle mass causes a progressive decrease in forced expiratory volume in 1 second by 6% to 8% per decade.
🍃Increases in pulmonary vascular resistance and pulmonary arterial pressure occur with age and may be secondary to decreases in cross-sectional area of the pulmonary capillary bed. Hypoxic pulmonary vasoconstriction is blunted in elderly individuals and may cause difficulty with one-lung ventilation.
Ref: Geriatric Anesthesia 2/e , Miller’s Anesthesia 7/e
#Physiology , #Anesthesia , #Geriatrics
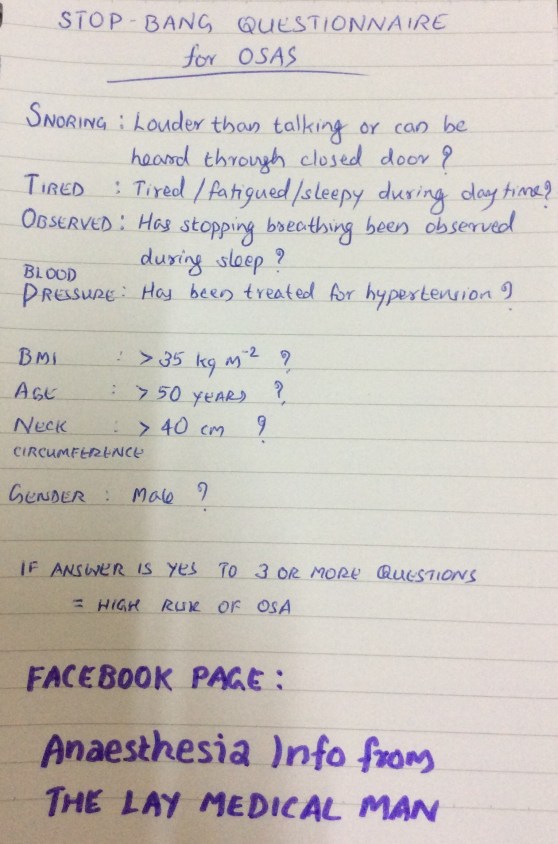
STOP BANG QUESTIONNAIRE FOR OSAS
NEGATIVE PRESSURE PULMONARY OEDEMA
# NPPO is associated with upper airway obstruction in a spontaneously breathing patient.
# It occurs in 0.05–0.1% of all general anaesthetic cases and laryngospasm has been reported as being the cause in 50% of cases.
#The clinical course is most frequently observed on emergence from anaesthesia where incomplete recovery from general anaesthesia increases the likelihood of the development of laryngospasm, but it has also been reported after airway obstruction with a foreign body and blockage and biting of tracheal tubes, hanging, and strangulation.
#Pulmonary oedema is typically described as developing within 2 min of the obstruction.
Once the airway is occluded, the spontaneously breathing patient will continue to generate negative intrathoracic pressure which will increase substantially as respiratory distress develops.
#There is an associated increase in sympathetic tone due to the stress of hypoxia and airway obstruction which increases SVR and elevates pulmonary artery pressure.
This is further exacerbated by hypoxic pulmonary vasoconstriction.
#The combination of these processes creates a pressure gradient across the capillary–alveolar membrane which favours the movement of fluid into the lung parenchyma.
#It is most common in younger patients, presumably because they are able to generate higher negative inspiratory pressures and, arguably, have a higher sympathetic tone and better cardiac function.
#The condition may resolve rapidly after definitive management of the airway obstruction, but in some cases, copious pulmonary oedema may form and it can be associated with pulmonary haemorrhage suggesting capillary membrane damage.
#After recognition of the cause of obstruction, the treatment required ranges from relatively modest support such as brief periods of CPAP for 2 h to positive pressure ventilation over a period of 24 h.#TheLayMedicalMan
Ref: Neurogenic pulmonary edema, Ronan O’Leary, Justin McKinlay, Contin Educ Anaesth Crit Care Pain (2011) 11 (3): 87-92.
http://feeds.feedburner.com/TheLayMedicalMan
A FEW POINTS ABOUT A SHARED LUNG
🔸In the pregnant patient, the respiratory function deviates from the normal
🔸There is increased CO2 production by the mother and the foetus; but mostly you see a respiratory alkalosis. Why?
🔸This is because the stimuli from the raised pCO2 levels and that by the respiratory stimulant, progesterone, sets the minute ventilation approximately 30% higher than the normal levels and this is more than what is needed to compensate for the increased CO2 production
🔸It is mainly the reduction in FRC (a reduction by 10-25% ; appears by 12th week ; is due to the reduced chest wall compliance ; lung compliance is normal ) which makes the patient more vulnerable to hypoxia.
🔸The alveolar diffusing capacity is reported to be normal during pregnancy
OSTEOGENESIS IMPERFECTA (OI) : POINTS OF ANESTHETIC RELEVANCE
🎲Bones and teeth are easy to break.The mandible is prone to fracture,but the facial bones are less so. Rib fractures have been reported. In the severest form, forced extension of the head during intubation carries a risk of vertebral fracture. Violent suxamethonium fasciculations can cause fractures.
🎲In the severe types of the disease,concern has been expressed that a blood pressure cuff may damage the humerus. Direct arterial monitoring has been suggested as an alternative
🎲Macrocephaly can be there. Airway problems may occur if the head is large, if there is macroglossia, or if the skeletal deformities are severe. If the head is large,a pillow placed under the chest may assist tracheal intubation.
🎲There is some evidence of hypermetabolism in this disease. Half of the patients have increased serum thyroxine levels. Hypermetabolic states, with hyperthermia, acidosis, sweating and cardiovascular instability, have been reported, but these are unrelated to Malignant Hyperthermia (MH).
🎲Surgery should be avoided in the pyrexial patient. Core temperature, oxygen saturation and ETCO2 should be monitored throughout surgery. Hyperthermia is reported to have responded to cooling alone.
🎲Platelet dysfunction may occur and produce a mild bleeding tendency, although the platelet count may be normal. But coagulopathies have been reported.
🎲Aortic and mitral valve insufficiency results from the defective connective tissue formation, but may be clinically inapparent. Sometimes cardiac surgery may be required
🎲Cranial developmental defects may cause brainstem compression, hydrocephalus, or vascular disruption. Softening of the basal portion of the occipital bone and upward movement of the cervical spine can combine to cause secondary basilar impression. Warning signs include cough, headache,vertigo, and trigeminal neuralgia.
🎲Those patients with kyphoscoliosis may have restrictive pulmonary defects. Sixty per cent have significant chest wall deformities. A thoracic scoliosis of more than 60 degrees will have severe effects on lung function, with a reduction in vital capacity to below 50%
🎲Although skeletal deformities and deranged coagulation may make regional anaesthesia technically difficult, successful and safe epidural anaesthesia has been reported in patients with OI.
Facebook page : Anesthesia Info from The Lay Medical Man
#anaesthesia , #TheLayMedicalMan , #Orthopedics , #OsteogenesisImperfecta , #fracture
ICTAL BRADYCARDIA AND ASYSTOLE : AN ENTITY ALL ANESTHESIOLOGISTS SHOULD KEEP IN MIND WHEN SEEING BRADYCARDIA IN A PATIENT WITH EPILEPSY
📌Ictal bradycardia/asystole is a poorly recognised cause of collapse late in the course of a typical complex partial seizure
📌It is important to identify ictal bradycardia as a potential harbinger of lethal rhythms, such as asystole, as this may be one important mechanism leading to sudden unexpected death in epilepsy (SUDEP)
📌Tachycardia is the most common rhythm abnormality occurring in 64–100% of temporal lobe seizures. Ictal bradycardia has been reported in less than 6% of patients with complex partial seizures
📌The ictal bradycardia syndrome occurs in mostly in patients with temporal lobe seizures.
📌It is believed that abnormal neuronal activity during a seizure can affect central autonomic regulatory centres in the brain leading to cardiac rhythm changes.
📌Ictal bradycardia/asystole may be unrecognised until documented during video-electroencephalograph (video EEG)–electrocardiogram (ECG) monitoring in those with refractory epilepsy, often in the context of pre-surgical evaluation
📌Other rhythm abnormalities which can occur are change in heart rate variability, ictal tachycardias and atrioventricular (AV) block
📌If sufficiently severe, the ictal-induced bradyarrhythmia temporarily impairs both cerebral perfusion and cortical function; the result has the dual effect of terminating the seizure, while at the same time triggering syncope with consequent loss of consciousness and postural tone. In essence, a complex partial seizure patient may manifest both seizure and syncope features during the same episode.
📌There are currently no guidelines on who should undergo further cardiovascular investigations ; dual chamber pacemaker implantation has been suggested as a treatment in the long term, for epilepsy patients who manifest this syndrome and suffer repeated falls; but there is not much mention in literature both about diagnosis and about pharmacological and non pharmacological interventions to counter such episodes when presenting as an emergency situation in the perioperative scenario , especially when the patient is under anesthesia.
#Neurology , #NeuroCriticalCare , #Anesthesia , #LayMedicalMan , #CriticalCare , #Epilepsy , #Cardiology , #CardiacAnesthesia
Reference: Ictal bradycardia and atrioventricular block: a cardiac manifestation of epilepsy; Salman S. Allana Hanna N. Ahmed Keval Shah Annie F. Kelly, Oxford Medical Case Reports, British Journal of Cardiology : Ictal Bradycardia and Asystole Associated with Intractable Epilepsy: A Case Series Elijah Chaila, Jaspreet Bhangu, Sandya Tirupathi, Norman Delanty; Ictal Asystole-Life-Threatening Vagal Storm or a Benign Seizure Self-Termination Mechanism? David G. Benditt, Gert van Dijk, Roland D. Thijs (Editorial:Circulation )