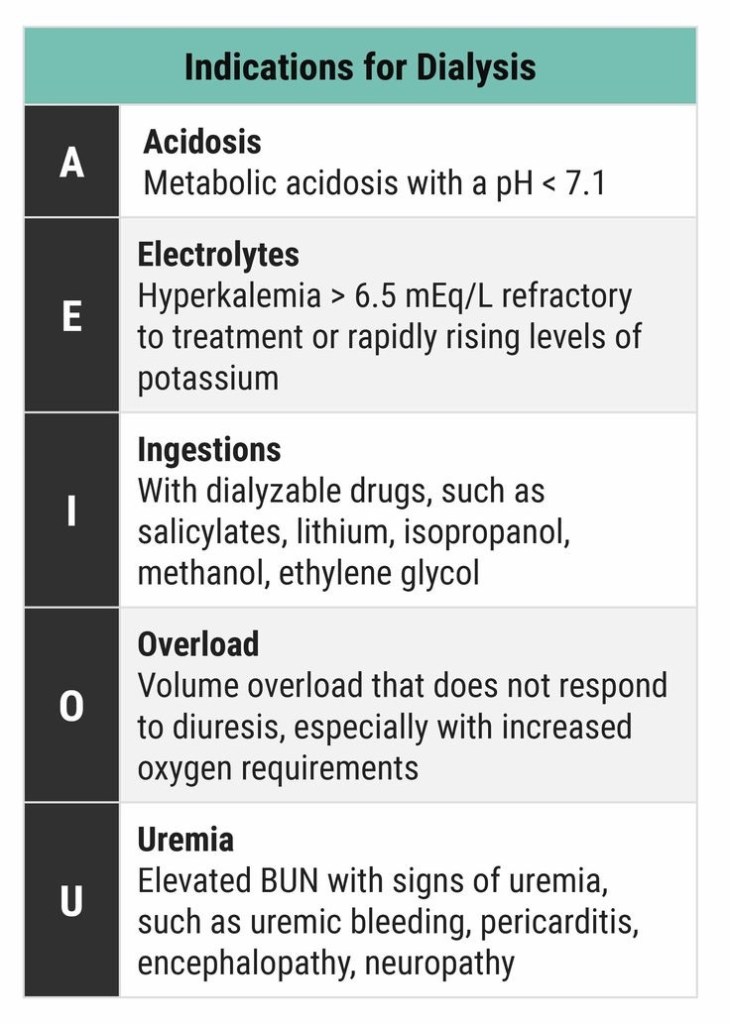
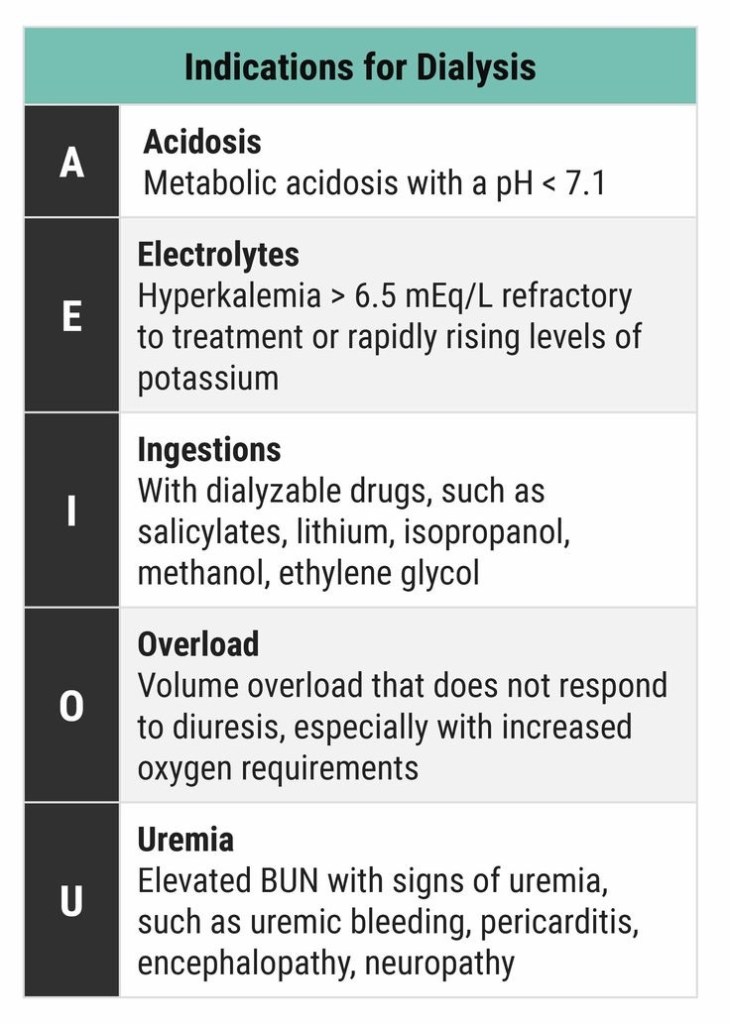
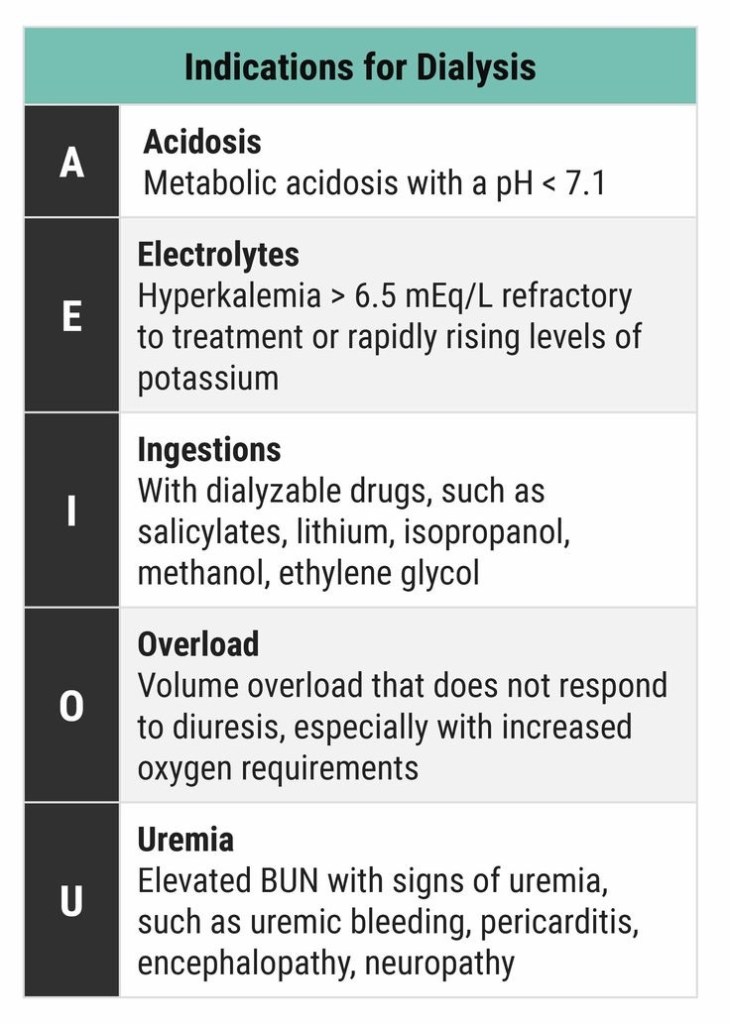
DIALYSIS INDICATIONS


Follow up the patient:
If voice is not improving: (Better to call the ENT Surgeon to do this-) Do a laryngoscopy and using any instrument, just give a mild pressure on aretynoid; usually it will fall back to correct position.
If speech is improving, advice VOCAL CORD ADDUCTION EXERCISES
Standing position.. Take a deep inspiration
and stop..and hold the breath.. this closes glottis..now strongly fall over and push against a wall…keep it for a few seconds.. Repeat this a few times.. This can force the aretynoid back to normal position by a stretching force… Usually voice is regained by this after 2 days..
Or lift heavy weights after deep inspiration (not for CAD patients)
Plus continue Speech Therapy
Problem occurs, when Aretynoid dislocates, and nobody attempts to relocate it, and it get fixed in that position..
Posterior tibial nerve :
Introduce the needle along the medial aspect of the Achilles tendon, at the level of the cephalic (towards head) border of the medial malleolus. Advance, in an anterior direction, towards the posterior border of the tibia (nerve lies just posterior to the posterior tibial artery).If paraesthesia is felt, inject 3-5ml LA. If not, advance to contact the tibia, withdraw 0.5cm and then inject 5-7ml LA.
Sural nerve :
Introduce the needle along the lateral border of the Achilles tendon at the level of the cephalic border of the lateral malleolus.Advance anteriorly towards the fibula.If parasthesia is felt inject 3-5ml LA. If not, inject 5-7ml LA as the needle is withdrawn. This gives subcutaneous infiltration from the Achilles tendon to the fibula.
Infiltration around the remaining three nerves can be performed from a single site. The needle is inserted 1cm lateral to the tendon of extensor hallucis longis (or just lateral to the anterior tibial artery, if palpable), at the level of the cephalic borders of the malleoli. This tendon is prominent on the dorsum of the foot, during extension of the big toe.
Deep peroneal nerve :
From the position described above, advance the needle posteriorly (i.e. at 90¡ to the skin). Inject 3-5ml LA deep to the fascia, on either side of the anterior tibial artery.
Superficial peroneal nerve :
After blocking the deep peroneal nerve, withdraw the needle to just stay in the skin.
Turn the needle towards the lateral malleolus and inject 5ml LA in a subcutaneous band between the lateral malleolus and the anterior border of the tibia. This should reach all the branches of this nerve.
Saphenous nerve :
Again withdraw the needle to just stay in the skin and turn the needle to point towards the medial malleolus.Infiltrate 5ml LA subcutaneously as the needle is advanced towards the medial malleolus. The great saphenous vein lies in this area, just antero-medial to the medial malleolus, in order to infiltrate around the vein, without causing damage, it may be necessary to make a further skin puncture lateral to the vein.
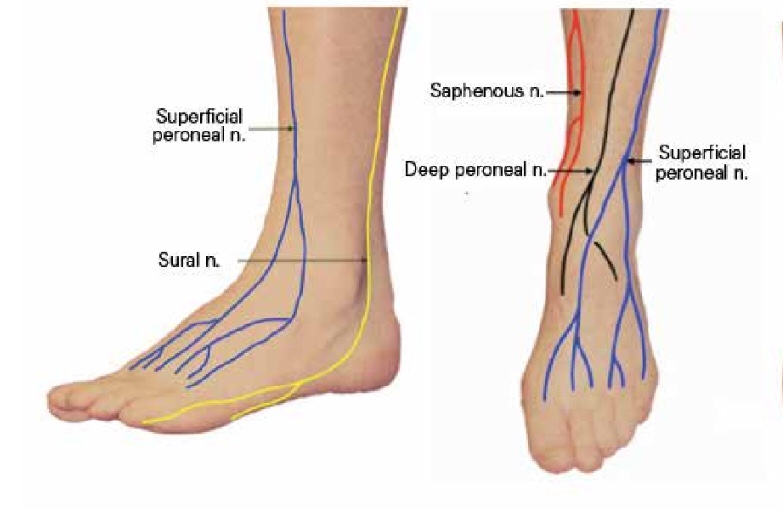
Image courtesy: Semantic Scholar
Ref: Quest to determine the ideal position of the central venous catheter tip D. K. Tempe1,* and S. Hasija, British Journal of Anaesthesia 118 (2): 148–50 (2017)
🚩#TURPsyndrome is diagnosed based on clinical signs, symptoms and biochemical findings
🚩The manifestations are due to hypervolemia, hyponatremia and due to the direct toxicity of the irrigation fluids like 1.5% glycine
▪️FACTORS INCREASING THE ABSORPTION OF THE IRRIGATION FLUID ( AND THUS CONTRIBUTING TO THE HYPERVOLEMIA )
🚩Long duration of the surgery: the irrigation fluid is absorbed at the rate of 20-30 mL/ min and so the volume absorbed increases with the duration of the surgery
🚩High pressure delivery of the irrigation fluid especially from a considerable height; the minimum height required for adequate flow should be used (usually 70 cms)
🚩Low venous pressures
🚩Excessive bleeding (= there are more open veins)
🚩Large prostate (>50g)
▪️CLINICAL FEATURES:
🚩Headache, Restlessness, Agitation, Confusion, Convulsions, Coma; pulmonary oedema may also set in. If patient is under general anesthesia, these symptoms will get masked.
▪️MANAGEMENT FROM SURGICAL SIDE:
🚩Coagulating bleeding points and terminating surgery as soon as possible.
▪️ANESTHETIC MANAGEMENT:
🚩Reduce / stop fluid administration. Diuretics may be required in the presence of pulmonary oedema
🚩Intubation to protect the airway and mechanical ventilation to support respiration may be required
🚩Anti-convulsants, if needed, to treat seizures
🚩Hypertonic saline should be considered for severe hyponatremia (<120 mmol L−1) or in the presence of severe neurological symptoms.
👉🏿N.B.- Central pontine myelinolysis or osmotic demyelinating syndrome (ODS) is more likely to occur with correction of serum Na greater than 8-12 mmol/day and in the setting of chronic hyponatremia (greater than 48 h)
👉🏿Faster rates of administration can potentially lead to central pontine myelinolysis. Treatment should stop once symptoms have resolved or the serum sodium is more than 125 mmol L−1. Such therapy is best delivered in a high-dependency environment.
🔻A template is given below for calculating the volume of hypertonic saline
#anesthesia , #urology ,#hyponatremia , #anaesthesiologist
