- A preoperative CT scan will show the site, severity, and extent of the airway compromise to assess the level and degree of obstruction.
- Assess the vocal cord function preoperatively
- Lung function tests to look for the extent of intrathoracic or extrathoracic obstruction.
- ECHO to rule out pericardial effusion and cardiac compression.
- Premedication with benzodiazepine is generally avoided if there is risk of airway compromise.
- Airway equipment—rigid bronchoscopy and difficult airway trolley, jet ventilation, cardiopulmonary bypass (CPB) should be there as standby. Femoro femoral bypass is the most common setup.
- COMPLICATIONS DUE TO MASS EFFECT OF THE TUMOUR:
- Vascular compromise—SVC Obstruction ( SVCO ) and pulmonary vessel obstruction
- Laryngeal nerve palsy
- Dysphagia
- STRIDOR and airway compromise may be an important symptom
- Inspiratory stridor (laryngeal)—obstruction above the level of glottis
- Expiratory stridor (tracheobronchial)—obstruction in the intrathoracic airways
- Biphasic stridor—obstruction between glottis and subglottis or a critical obstruction at any level
- Sometimes you may have to go for a microlaryngoscopy tube (MLT)
- TAKE CARE:
- Aim to avoid worsening of cardiac compression, airway occlusion, and SVC obstruction.
- IV cannula in the lower extremity
- Induction in sitting position (semi Fowler’s position)
- Inhalational (preferred choice) or IV induction agent titrated to effect
- Choose spontaneous ventilation with LMA
- Awake fibreoptic technique if intubation is necessary with a reinforced smaller calibre and longer endotracheal tube
- Postoperative airway obstruction due to airway oedema, tracheomalacia, and bleeding warrant the need for awake extubation in ITU. The following steps would aid in an uneventful extubation:
- Test for leak around the endotracheal tube cuff.
- Administer dexamethasone or chemo radiotherapy in sensitive tumours to shrink size of tumour.
- Use adrenaline nebulisers.
- Extubate over airway exchange catheters.
- SVCO: challenges during anaesthesia
- Need for supplemental oxygen
- Orthopnoea—induction in the sitting-up position
- IV cannula in the lower extremity
- Airway oedema
- Mucosal bleeding
- Laryngeal nerve palsy
- Haemodynamic instability due to decreased venous return
- OTHER CONCERNS
- General anaesthesia, causes loss of intrinsic muscle tone, decreased lung volumes, and decreased transpleural pressure gradient
- Positive pressure ventilation, can precipitate severe hypotension and also increases intrathoracic tracheal compression
- Coughing, as it can cause complete airway obstruction by positive pleural pressure, increasing intrathoracic tracheal compression
- Following gas induction, the patient stops breathing and if you are unable to ventilate her: Follow difficult or failed intubation guidelines. But cricoid puncture and emergency tracheostomy are futile if the level of airway obstruction is at the intrathoracic tracheobronchial tree: Try a change in position—lateral, sitting up, or prone—to decrease the mechanical effect of the tumour. Avoid positive pressure ventilation for fear of luminal closure. Low-frequency jet ventilation with Sander’s injector or high-frequency translaryngeal jet ventilation with Hunsaker’s catheter is one option. CPB bypass and ECMO to restore oxygenation when other measures fail.
- Following chemotherapy in ICU, if patient develops hyperkalemia, Tumour Lysis Syndrome should be there in the differential diagnosis
- ALSO NOTE
- During inspiration, the intrathoracic airways expand along with the expanding lungs. In contrast, the extrathoracic airways diminish in caliber during inspiration due to their intraluminal pressure being lower than the atmospheric pressure. The reverse happens during expiration.
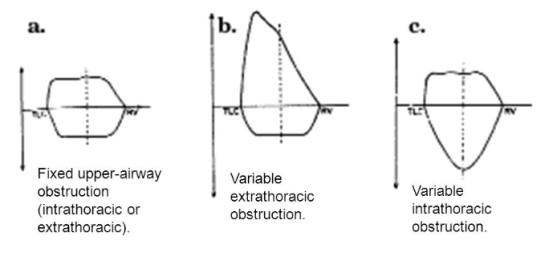
- Flow volume loop in upper-airway obstruction:
- Fixed lesions [extrathoracic or intrathoracic] are characterized by lack of changes in caliber during inhalation or exhalation and produce a constant degree of airflow limitation during the entire respiratory cycle. Its presence results in similar flattening of both the inspiratory and expiratory portions of the flow-volume loop
- Variable lesions are characterized by changes in airway lesion caliber during breathing. Depending on their location (intrathoracic or extrathoracic), they tend to behave differently during inhalation and exhalation.
- In the case of an extrathoracic obstructing lesion, during inspiration, there is acceleration of airflow from the atmosphere toward the lungs, and the intraluminal pressure decreases with respect to the atmospheric pressure due to a Bernoulli effect, resulting in the limitation of inspiratory flow seen as a flattening in the inspiratory limb of the flow-volume loop. During expiration, the air is forced out of the lungs through a narrowed (but potentially expandable) extrathoracic airway. Therefore, the maximal expiratory flow-volume curve is usually normal.
- Variable intrathoracic constrictions expand during inspiration, causing an increase in airway lumen and resulting in a normal-appearing inspiratory limb of the flow-volume loop. During expiration, compression by increasing pleural pressures leads to a decrease in the size of the airway lumen at the site of intrathoracic obstruction, producing a flattening of the expiratory limb of the flow-volume loop
Category Archives: Exams EDAIC FRCA
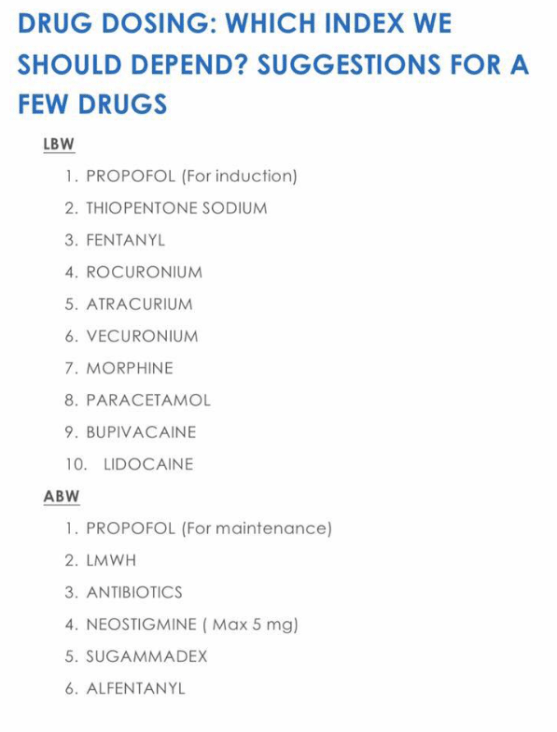
TOTAL BODY WEIGHT [TBW] , LEAN BODY WEIGHT [LBW], IDEAL BODY WEIGHT [IBW] &ADJUSTED BODY WEIGHT ; THEIR IMPLICATIONS IN Anesthesia AND CriticalCare
Drug administration in obese patients is difficult because recommended doses are based on pharmacokinetic data obtained from individuals with normal weights
With increasing obesity, fat mass accounts for an increasing amount of TBW, and the LBW/TBW ratio decreases
TBW is defined as the actual weight
IBW is what the patient should weigh with a normal ratio of lean to fat mass
IBW can be estimated from the formula: IBW (kg) = Height(cm) − x ( where x = 100 for adult males and 105 for adult females).
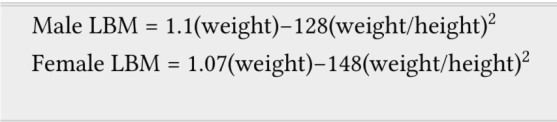
LBW is the patient’s weight , excluding fat
Male LBW = 1.1(weight)-128(weight/height)^2 (Weight in Kg and Height in cm)
Female LBW = 1.07 (weight) -148 (weight/height)^2
Regardless of total body weight, lean body weight rarely exceeds 100 kg in men and 70 kg in women
Below IBW, TBW and LBW are similar.
Adjusted body weight (ABW) Takes into account the fact that obese individuals have increased lean body mass and an increased volume of distribution for drugs.
It is calculated by adding 40% of the excess weight to the IBW : ABW (kg) = IBW (kg) + 0.4 [TBW (kg)]
Drugs with weak or moderate lipophilicity can be dosed on the basis of IBW or more accurately on LBW. These values are not same in obese; because 20–40% of an obese patient’s increase in TBW can be attributed to an increase in LBW. Adding 20% to the ‘estimated IBW based dose’ of hydrophilic medication is sufficient to include the extra lean mass. Non-depolarizing neuromuscular blocking drugs can be dosed in this manner.
In morbidly obese patients, the induction dose of propofol can be calculated on IBW.
In case of midazolam, prolonged sedation can occur from the larger initial dose needed to achieve adequate serum concentrations. #TheLayMedicalMan
Remifentanil dosing regimens should be based on IBW or LBW and not on TBW.
When using succinylcholine in obese adults or adolescents, dosage should be calculated on TBW
The antagonism time of neostigmine has been shown to be independent of TBW and BMI. Therefore, TBW can be used to calculate the dose.
Ref:Association of Anaesthetists of Great Britain and Ireland. Peri-operative management of the obese surgical patient 2015. Anaesthesia 2015, 70, pages 859–876.
ROBOTIC 🤖 PROSTATECTOMY: Anesthesia CONCERNS
FACTS ABOUT THE SURGERY
There is a master console; surgeon sits here & controls the robotic surgical manipulator, once it has been docked
Robot is bulky and is positioned over the chest and abdomen
Patient is positioned in lithotomy with a steep Trendelenberg tilt
Needs immobility of the patient till the robot is undocked
Table position should not be altered until the surgical instruments are disengaged
Discharge may occur as early as within 24 hours after surgery
ADVANTAGES
Better continence & erectile function
Less pain and hence less analgesic requirements
Less blood loss
Shorter hospital stay
ANESTHESIA CONCERNS
Since immobility is very important, it can be established by continuous infusion of a non depolarizing muscle relaxant
As the procedure may take long time, it’s better to use agents with rapid offset
Because patient is positioned in steep head-down position
Ensure pressure points are protected adequately
Fluids are infused cautiously to reduce chances of cerebral and laryngeal oedema ( N.B.: Rule out cerebral oedema in case of delayed emergence )
As the position of the robot interferes with resuscitation, prior practice-drills and good communication are necessary to manage such a situation effectively
Epidural analgesia, if at all required, are used only postoperatively, as the steep head-down position will increase the risk of high block
Reference: Irvine M, Patil V. Anaesthesia for robot-assisted laparoscopic surgery. Contin Educ Anaesth Crit Care Pain. 2009; 9(4): 125–129.
#ProstateSurgery , #RoboticSurgery , #anaesthesia , #perioperative
WHEN VENTILATOR GIVEs ALARM & SHOWS ‘PATIENT-DEMAND IS HIGH’ : Troubleshooting the Ventilator
Check for causes:
Increased airway resistance- if so give bronchodilators
Anxiety–> increased RR + muscle tension–> increased airway resistance –> increased demand: Optimise sedation
Check for leaks in circuit and correct
If flow rate seems too low: Set higher inspiratory flow rate or reduce inspiratory time especially if patient is showing tachypnea
If Tidal volume or RR set too low: Increase it
Double triggering or breath stacking can happen if inspiratory time set is lower compared to that of the patient and ventilatory demand is high: Try increasing the inspiratory time or change to pressure control modes
NB:
Peak Inspiratory Pressure high with normal Plateau Pressure = it’s Increased airway resistance
Both (a)Peak Inspiratory Pressure and (b)Plateau Pressure are high and (a)-(b) is normal= it’s reduced compliance or auto peep
#CriticalCare , #MechanicalVentilation ,#VentilationBasics , #Ventilation , #anesthesia , #anesthesiologist , #ICUnurse , #ICUdoctor , #ICU
MECHANICAL VENTILATION FACTS
LOW FLOW Anesthesia
Low flow anesthesia allows for economy of volatile anesthetics, makes possible heating and humidification of gases and reduces environmental pollution
Sodalime contains 94% Calcium hydroxide, 5% Sodium hydroxide and also Potassium hydroxide, Silica and dying agent
CO2 + 2NaOH –> Na2CO3 + water + heat
Na2CO3 + Ca(OH)2 –> 2NaOH + CaCO3
..this sequence gets back Sodium hydroxide
1 Kg of Sodalime can absorb >120 L of CO2
Carbon monoxide which is a byproduct of protein metabolism can accumulate in the system, but levels are <4%
If there is intoxication by alcohol or poisoning by Carbon monoxide or severe diabetic ketosis, alcohol or CO or acetone from the expired gases, will recirculate and accumulate inside the system; so low flow anesthesia is contraindicated in such states
Prolonged anesthesia with sevoflurane may generate Compound A inside the system, which can cause acute tubular necrosis in rats at concentrations around 250 ppm, a dose that is nearly 200 times seen in clinical practice. So any proteinuria, glycosuria or enzymuria which does develop in such a context has not been shown to have any clinical significance, even in patients with pre-existing renal disease
Reference: Al-Shaikh B, Stacey S. Essentials of Anaesthetic Equipment, 2nd edn. Edinburgh: Churchill Livingstone, 2002; pp. 74–9 . Nunn G. Low-flow anaesthesia. Contin Educ Anaesth Crit Care Pain 2008; 8: 1–4.
POSTOPERATIVE VISUAL LOSS
Corneal abrasion is the most common ocular complication after general anesthesia
Ischemic Optic neuropathy (ION) and Central Retinal Artery Occlusion (CRAO) are the commonest causes for postoperative visual loss
ISCHEMIC OPTIC NEUROPATHY (ION)
More common among the two
Most often seen after prolonged surgery in prone position
Venous congestion–> Raised Intra Ocular Pressure (IOP) due to Raised Intra Orbital Pressure –> Intra Orbital ‘Compartment Syndrome’
Hypotension, Diabetes, Vascular disease, Smoking etc also may be important in the etiopathogenesis
Treatment:
Reduce optic nerve edema as it passes through posterior scleral foramen with steroids and mannitol
Optimal oxygen delivery by ensuring normal blood pressure and hematocrit
Clear all obstruction to venous drainage
Chance of visual recovery is less
CENTRAL RETINAL ARTERY OCCLUSION (CRAO)
External pressure on eye and embolism are risk factors
An echocardiogram and carotid ultrasound may help us to find an embolic source
Reference: White E, David DB. Care of the eye during anaesthesia and intensive care. Anaesth Intens Care Med. 2007; 8(9): 383–386.
SUGAMMADEX & DRUG INTERACTIONS
Sugammadex acts by forming a complex with steroidal Neuro Muscular Blocking Agents such as rocuronium and vecuronium and reduces their concentrations in the neuromuscular junction.
Because of its inert structure, direct drug interactions are rarely expected with sugammadex. Two types of drug interactions may occur with sugammadex by displacement or capturing.
Drugs interacting with sugammadex by displacement : toremifene, fusidic acid, and flucloxacillin, could potentially affect the efficacy of sugammadex due to rocuronium
or vecuronium being displaced from sugammadex.
Capturing interactions may occur if sugammadex binds with other drugs (i.e., hormonal contraceptives), and reduces their free plasma concentration. In addition, sugammadex might have decreased efficacy for rocuronium or vecuronium due to it binding with another drug.
Cyclodextrins have been reported to form inclusion complexes with other compounds.
In an in vitro experimental model of functionally innervated human muscle cells Rezonja et al. found that dexamethasone led to a dose-dependent inhibition of sugammadex reversal; but Ersel Gulec et al, who investigated the clinical relevance of the interaction between dexamethasone and sugammadex in humans failed to demonstrate any inhibitory effect of dexamethasone (0.5 mg/kg) on the reversal time of sugammadex in children.
N.B.(DO YOU KNOW?): It is clearly demonstrated that dexamethasone attenuates rocuronium-induced neuromuscular blockade when administered 2 to 3 hours before the induction of anesthesia; but not when dexamethasone is given at induction
Reference: The Effect of Intravenous Dexamethasone on Sugammadex Reversal Time in Children Undergoing Adenotonsillectomy; Ersel Gulec, Ebru Biricik, Mediha Turktan, Zehra Hatipoglu and Hakki Unlugenc, April 2016 • Volume 122 • Number 4, anesthesia-analgesia
ANTIDEPRESSANTS; AS ANALGESIC Vs AS ANTIDEPRESSANT
The tricyclic antidepressants prevent the reuptake of monoamines, including serotonin and noradrenaline, as both pathways are important in the pain propagation. So the mixed reuptake drugs work better than more selective drugs like SSRIs
But serotonin-noradrenaline reuptake inhibitor antidepressants (SNRIs), for example, venlafaxine & duloxetine and the atypical antidepressant group, such as bupropion and mirtazapine are also effective for some chronic pain conditions and are increasingly used because of their improved tolerability
The superiority of tricyclics, particularly clomipramine and amitriptyline, in the management of pain may also be explained by their additional action on sodium channels blockade ( which is an action that SNRIs do not exhibit.)
The dose of amitriptyline to treat pain is much lower when compared to that needed to treat depression
The analgesic action has a faster onset, whereas antidepressant action takes weeks to start
The sedative action of tricyclic antidepressants are helpful in treating the sleep disturbances associated with neuropathic syndromes. Nortriptyline is less sedative than amitriptyline.
#antidepressants , #analgesics , #PainManagement , #ChronicPain
Reference: Medscape, Pharmacogenetics and Analgesic Effects of Antidepressants in Chronic Pain Management, Frédérique Rodieux; Valérie Piguet; Patricia Berney; Jules Desmeules; Marie Besson, Personalized Medicine. 2015;12(2):163-175.
Ryder S A, Stannard C F. Treatment of chronic pain: antidepressant, antiepileptic and antiarrhythmic drugs. Contin Educ Anaesth Crit Care Pain 2005; 5: 18–20 .
A TRAVELOGUE: The long journey of Insulin
Insulin is produced by beta cells of islets of Langerhans.
It is produced from the pro hormone, ‘preproinsulin’ in endoplasmic reticulum. A portion of the structure is cleaved off and the remaining portion is folded with the help of C-peptide to form ‘proinsulin’
The C-peptide portion is then removed to form Insulin
This active Insulin is transported via Golgi apparatus to cytoplasmic granules for exocytosis into plasma
Insulin then binds with its receptor on Insulin sensitive cells
Insulin receptor is a tetramer consisting of 2 alpha & 2 beta units.
Insulin binds to the alpha unit on the cell membrane, while the beta unit, which spans the cell membrane activates tyrosine kinase and the second messenger system
This activates cytoplasmic vesicles containing transport molecules
The vesicles fuse with the cell membrane to incorporate the transport molecules into the cell membrane, which facilitate the transport of glucose into the cell.
MNEMO> MECHANISM OF ACTION: INSULIN Vs GLUCAGON
Insulin binding to the receptor activates an intracellular second-messenger system via tyrosine kinase.
Glucagon binding to its receptor activates a G-protein second-messenger system via adenylyl cyclase.
“Insulin is TricKy”
“Glucagon is ACcurate”






