| Bedside Test | Procedure | Normal / Reassuring Value | Clinical Significance (Red Flag) |
|---|---|---|---|
| Clinical Assessment | Observe for signs of respiratory distress and bulbar weakness (speech, swallowing). | No accessory muscle use, effortless breathing, strong cough, clear voice. | Tachypnea, accessory muscle use, paradoxical breathing, weak “boggy” cough, slurred/fading voice. |
| Vital Capacity (VC) | Patient takes a maximal inhalation and exhales fully into a bedside spirometer. | > 20 mL/kg (ideal body weight) | < 15-20 mL/kg, or a declining trend during the breathing trial. |
| Negative Inspiratory Force (NIF) / MIP | Patient makes a maximal inspiratory effort against an occluded airway for ~20 seconds. | More negative than -30 cm H₂O | Less negative than -30 cm H₂O (e.g., -25, -20), or a worsening trend. |
| Single Breath Count | Patient takes a deep breath and counts aloud steadily (e.g., “1-one-thousand, 2-one-thousand…”). | > 25 | < 15-20. Indicates severely reduced vital capacity. |
| Head Lift Test | Patient lies supine and lifts their head off the bed, holding the position as long as possible. | > 30 seconds | < 20 seconds. Correlates with significant diaphragmatic weakness. |
| Breath-Holding Time | After a maximal inhalation, the patient holds their breath for as long as possible. | > 30 seconds | < 20 seconds. Suggests poor respiratory reserve. |
Category Archives: Neurocritical Care
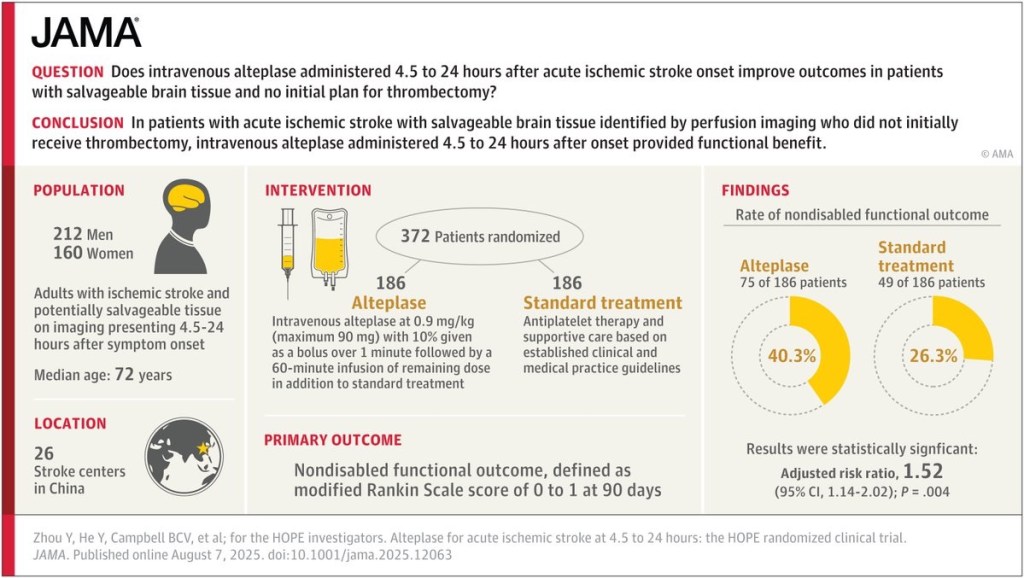
Does intravenous alteplase administered 4.5 to 24 hours after acute ischemic stroke onset improve outcomes?