
STEROID EQUIVALENT DOSES



Increased blood sugars 4-6 h prior to delivery leads to increased rates of hypoglycemia in the neonate. A maternal blood glucose value of more than 180 mg/dl has been conclusively proven to be associated with high risk of neonatal hypoglycemia.
The American College of Obstetrics and Gynecology and the American College of Endocrinology recommends maintenance of blood glucose between 70 and 110 mg/dl during labor (3.9-6.1 mmol/L) this goal is the same irrespective of whether the women has type 1 diabetes, type 2 diabetes or GDM.
The hepatic glucose supply is sufficient during the latent phase of labor, but during the active phase of labor the hepatic glucose supply is depleted so calorie supplementation is required.
During labor in a case with GDM controlled only on life-style modification, it is not compulsory to monitor blood sugars periodically and monitoring once in every 4-6 h is sufficient during labor
In patients on insulin it is mandatory to monitor the blood sugar every 2-4 h during the latent phase, every 1-2 h during the active phase
In patients for whom cesarean is planned, it always preferred to do the procedure early morning.
Patient needs to take her usual night dose of intermediate-acting insulin and the morning dose of insulin has to be withheld and patient needs to be kept nil by mouth.
If surgery is delayed it is needed to start basal and corrective regimen (DNS with short acting insulin) with one-third of the morning intermediate insulin dose with a 5% dextrose infusion to avoid ketosis. Blood glucose has to be monitored second hourly and if required subcutaneous dose of corrective dose of short acting insulin to be given.
After delivery, the requirement of insulin shows a sharp decline and in GDM it is advisable to continue the monitoring to see if the sugars have become normal in the postpartum period
In cases with type 1 and type 2 DM it is prudent to decrease the dose of insulin by 20-40% of the pregnancy dose as the requirement of insulin during lactation is less. During the breast-feeding, sometimes the requirement of insulin can fall drastically and these women may develop hypoglycemia, so the dose of insulin needs to be adjusted accordingly
Reference: ACOG Practice Bulletin, 137, 2013
Indian Journal of Endocrinology and Metabolism: Peripartum management of diabetes, Pramila Kalra and Manjunath Anakal
Rotation of an opioid, secondary to uncontrolled pain requires equianalgesic doses.
If you are rotating an opioid secondary to toxicity, it requires a dose 30-50% lower than the equivalent dose of the second opioid. This is because of incomplete analgesic cross-tolerance.
Thirty percent of patients who are on opioids need an alternative route, as in severe nausea or mucositis.
Once toxicity occurs, before doing rotation, consider treating side effects, lowering the dose of the current opioid(if pain is controlled), and use of adjuvant analgesics.
Whenever we start or titrate opioid dose, always consider the pharmacokinetic alterations due to age, comorbid conditions, gender, other simultaneously administered medications, and organ failure etc
Opioids that are partial agonists have less analgesia per dose increment at higher doses than full agonists or opioids with high intrinsic efficacy (e.g., methadone); therefore, equianalgesic ratios will change with dose.
Rotating to a new opioid before reaching steady-state of the first opioid is pharmacologically meaningless.
Rotation in the setting of organ dysfunction is dangerous even if we use the recommended doses from equianalgesic tables.
Note that, opioids may worsen intestinal colic. Dexamethasone, glycopyrrolate, or octreotide are better options for such pains.
Opioid-induced toxicity takes some time to resolve. If symptoms related to toxicity are persisting after rotation, it can be because of slow clearance of the first opioid and not the new opioid.
Be cautious while rotating between short and long-acting opioids and do it in a careful way, so as to avoid withdrawal or overdosing.
Reference: Opioid Equianalgesic Tables: Are They All Equally Dangerous? Philip E. Shaheen, Declan Walsh, Wael Lasheen, Mellar P. Davis and Ruth L. Lagman (Journal of Pain and Symptom Management, Vol. 38 No. 3 September 2009)
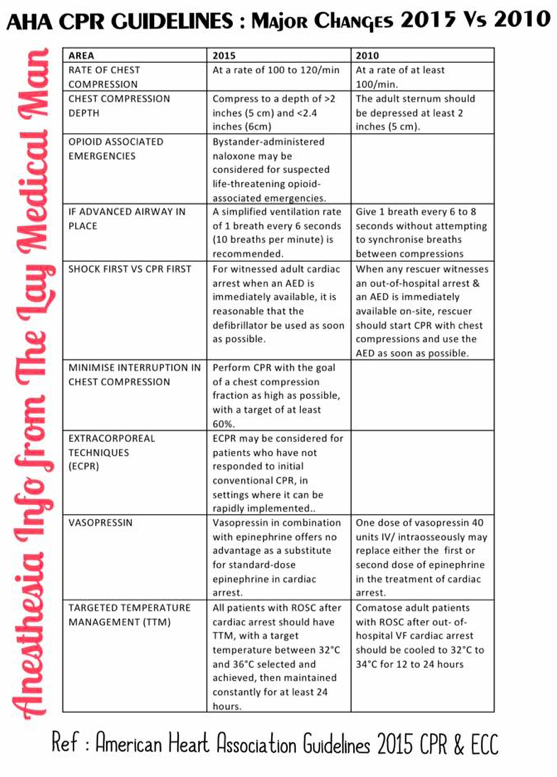
Sorry. Please note that the DATA IN THE FIRST TWO COLUMNS HAVE TO BE INTERCHANGED. i.e. Regarding the RATE and DEPTH of compression, “at least” specification has come in the 2015 GUIDELINES
What’s the problem, if we place the temperature probe in upper 1/3rd or 2/3rd of the esophagus?
Esophageal temperature should be taken from the lower third of the oesophagus; placed above this level, the probe may under-read due to cooling effect of inspired gases. It gives a good estimate of cerebral blood temperature.
What’s the advantage of nasopharyngeal temperature measurement over oesophageal measurement?
The nasopharyngeal temperature probe is placed just behind the soft palate. The advantage is that it is more accessible compared to the oesophageal temperature measurement. The disadvantage is that it is less accurate in representating the core temperature.
What are the advantages of measurement of temperature @ Tympanic membrane?
The tympanic membrane provides an accurate representation of hypothalamic temperature. It is less invasive, has a short response time and correlates well with oesophageal temperature. But it does not allow continuous measurements.
What is the best method for CONTINUOUS measurement of core temperature?
Blood temperature measurement using a pulmonary artery flotation catheter
What are the factors reducing the accuracy of Rectal temperature measurement?
Rectal temperature is influenced by heat generated from gut flora, the cooling effect of blood returning from the lower limbs and the insulation of the probe by faeces. It is normally about 0.5–1.0 ° C higher than core temperature and has a slow response time.
Can you say an e.g. of utilising the temperature gradients existing between different sites of the body for clinical advantage?
The gradient between a skin temperature and a core temperature can be used as a marker of peripheral perfusion.
Train of four (TOF)
four stimuli {T1-T4} are given at a frequency of 2 Hz (0.5 sec between the stimuli)
Each stimulus in the train causes the muscle to contract and the ‘fade’ in the response allow us to evaluate the neuro muscular blockade
The ratio T4:T1 ( i.e. Dividing the amplitude of the fourth response by the amplitude of the first response ) indicates the degree of neuromuscular block.
Non-depolarizing NMBAs produce a decrease in magnitude of the first twitch compared with a pre-relaxant stimulus, and a progressive reduction in magnitude of T1–T4.
The number of elicited twitches indicates the degree of receptor occupancy.
Disappearance of T4, T3, T2, T1 corresponds to 75%, 80%, 90% and 100% occupancy.
With recovery of neuromuscular function the twitches appear in the reverse order.
Accepted values for TOF count are:
1 twitch for tracheal intubation
1–2 twitches during established anaesthesia
3–4 twitches before reversal of neuromuscular blockade is attempted.
Double burst stimulation
Consists of two bursts ( the duration of each square wave impulse in the burst is 0.2 sec ) at 50 Hz with each triple burst separated by 750 ms.
DBS with 3 impulses in each of the two tetanic bursts is commonly used
These manifest visually as two separate stimuli (T1 and T2).
The ratio is related to the TOF ratio and is easier for the operator to interpret reliably.
Used under light paralysis where train of four ratio is difficult to distinguish
Post-tetanic Count (PTC)
PTC is used when there is no response to TOF stimuli and also when we want to eliminate sudden movements of the patient completely as during ophthalmic and neurosurgery
Uses tetanic stimulation at 50 Hz for 5 s to mobilize presynaptic ACh (to ‘kick start’ the nerve under deep paralysis) .
After a recovery time of 3 sec , it’s followed by 20 pulses at 1-2 Hz twitch stimulation
The number of twitches generated (i.e. the post-tetanic count) reflects the degree of neuromuscular blockade.
Shows fade response earlier than train of four
Used under deep paralysis to estimate time to recovery
#nmb ,#anesthesia ,#anaesthesia , #CriticalCare , #NerveStimulator , #AnesthesiaTechnician ,#NurseAnesthetist ,#AnesthesiaEquipment,#Biomedical ,#BiomedicalEquipment
Reference: frca.uk Anesthesia Monitoring Techniques , Miller’s Anesthesia , 7/e
Supplementary oxygen to all hypoxaemic patients with acute severe asthma to maintain an SpO2 level of 94-98%
Nebulisers for giving nebulised β2 agonist bronchodilators should preferably be driven by oxygen. A flow rate of 6 l/min is required to drive most nebulisers
High-dose inhaled β2 agonists as first line agents in patients with acute asthma. Repeat doses of β2 agonists at 15–30 minute intervals or give continuous nebulisation of salbutamol at 5–10 mg/hour (requires appropriate nebuliser) if there is an inadequate response to initial treatment. Higher bolus doses, for example 10 mg of salbutamol, are unlikely to be more effective (2.5–5 mg salbutamol in children >2 years).
There is no evidence for any difference in efficacy between salbutamol and terbutaline. Nebulised adrenaline (epinephrine), a non-selective β2 agonist, does not have significant benefit over salbutamol or terbutaline.
Add nebulised ipratropium bromide (0.5 mg 4-6 hourly) to β2 agonist treatment for patients with acute severe or life-threatening asthma or those with a poor initial response to β2 agonist therapy. ( 250 micrograms/dose in children >2 years).
Consider giving a single dose of IV magnesium sulphate (1.2-2 g IV infusion over 20 minutes) to patients with acute severe asthma who have not had a good initial response to inhaled bronchodilator therapy.
Nebulised magnesium is not recommended for treatment in adults with acute asthma. Consider adding 150 mg magnesium sulphate to each nebulised salbutamol and ipratropium in the first hour in children >2 years with a short duration of acute severe asthma symptoms presenting with an oxygen saturation less than 92%.
Routine prescription of antibiotics is not indicated for patients with acute asthma.
SECOND LINE TREATMENT OF ACUTE ASTHMA
Consider early addition of a single bolus dose of intravenous salbutamol (15 micrograms/kg over 10 minutes) in a severe asthma attack where the patient has not responded to initial inhaled therapy.
Consider aminophylline for children >2 years with severe or life-threatening asthma unresponsive to maximal doses of bronchodilators and steroids. A 5 mg/kg loading dose should be given over 20 minutes with ECG monitoring (omit in those receiving maintenance oral theophyllines) followed by a continuous infusion at 1 mg/kg/hour. Measure serum theophylline levels in patients already receiving oral treatment and in those receiving prolonged treatment.
NOTE:
Give steroids in adequate doses in all cases of acute asthma attack.
Prednisolone 40–50 mg daily or parenteral hydrocortisone 400 mg daily (100 mg six-hourly in adults and 4 mg/kg repeated four hourly in children >2 years ) are as effective as higher doses. Continue prednisolone 40–50 mg daily for at least five days or until recovery. ( In children >2 years, treatment for up to three days is usually sufficient).
Following recovery from the acute asthma attack steroids can be stopped abruptly. Doses do not need tapering provided the patient receives Inhaled Corticosteroids
In adults with an acute asthma attack, i.v. aminophylline is not likely to result in any additional bronchodilation compared to standard care with inhaled bronchodilators and steroids. Side effects such as arrhythmias and vomiting are increased if Iv aminophylline is used
Heliox is not recommended for use in patients with acute asthma outside a clinical trial setting
Although theoretically furosemide may produce bronchodilation, a review of three small trials failed to show any significant benefit of treatment with nebulised furosemide compared to β 2 agonists
vHLD usually presents in young adults with cerebellar, medullary or spinal haemangioblastomas, retinal angiomatosis, renal cell carcinoma and phaeochromocytoma
The frequency of phaeochromocytomas is 7–20%
About 25% of patients with CNS haemangioblastomas subsequently turn out to have vHLD.
Erythrocytosis and a high haematocrit are common and has to be searched for.
Surgery for one manifestation of the disease may be complicated by the presence of an undiagnosed #phaeochromocytoma. In this situation, pharmacological control of phaeochromocytoma should get more priority and surgery may have to be carried out in two stages
Spinal Anaesthesia may be dangerous in the presence of an undiagnosed cerebral or spinal tumour. Another point is, spinal cord haemangioblastomas can occur at more than one level. An MRI if already done, can help us to take a proper decision.
Pregnancy may worsen the disease, by increasing the vascularity of tumours. Urgent and life saving neurosurgical intervention may become necessary: for e.g. when a spinal tumor bleeds, when a tumor obstructs CSF flow and causes acute hydrocephalus. Sometimes elective procedures like removal of a phaeochromocytoma which became evident during pregnancy has to be removed. It may become necessary to carry out these procedures during pregnancy or along with a Caesarean section.
Surgery may be required for more than one lesion at the same time.
So careful assessment should be made for lesions other than the one for which anaesthesia is required, and in particular for any symptoms and signs of cerebral, cerebellar or spinal cord tumours and phaeochromocytoma.
In the situation in which two lesions are present, decisions may have to be made as to whether to operate simultaneously or separately . During pregnancy the management of the delivery must be carefully planned in advance.
Although 24-h urinary screening for catecholamines can be performed, plasma normetanephrines and metanephrines are the most sensitive tests for detecting phaeochromocytomas in patients with family predisposition
Reference: Anaesthetic management of a patient with von Hippel–Lindau disease: a combination of bilateral phaeochromocytoma and spinal cord haemangioblastoma. European Journal of Anaesthesiology 13: 81–3. , Anesthesia Databook, 3rd edition
NICE published guidelines in 2006, revised in 2011.
Step 1 : Choose either an ACE inhibitor, a thiazide diuretic or a calcium channel antagonist (A, D and C).
An ACE inhibitor is more effective as first-line therapy in younger patients (< 55 years ) and Caucasians.
Diuretics or calcium channel blockers are better in older patients and African / Caribbean patients of any age.
This trial of step 1 is run on for 4 weeks, and if blood pressure is not controlled, the opposite agent is added in:
Step 2 : An ACE inhibitor is added to a diuretic (A + D) or calcium channel antagonist (A + C), or vice versa.
Step 3 : Ongoing poor control is then managed by the addition of the third agent (A + C + D).
Step 4 : If a patient is established on triple therapy, and still not well controlled, they are probably aldosterone sensitive, so spironalactone would be a wise option.
National Institute for Health and Clinical Excellence. Hypertension: Clinical Management of Primary Hypertension in Adults. NICE Clinical Guideline 127, August 2011.
Entonox is Nitrous oxide mixed 50:50 with oxygen
It provides analgesia with maintenance of consciousness.
Usually administered via a demand valve for self administration.
Takes 30 seconds to act and continues for approx. 60 sec after inhalation has stopped
For optimum effect inhalation should start when the contraction tightens. This will co-ordinate the maximal effect with the central painful part of the contraction.
20% N20 is equivalent to 15 mg of subcutaneous morphine.
The optimal analgesic concentration was found to be 70% but some mothers lost consciousness at this concentration
50% N20 in oxygen is safer and this has become standard now
Entonox is the BOC trade name for this gas mixture.
Poynting effect
The Poynting effect involves the dissolution of gaseous O2 when bubbled through liquid N2O, with vaporisation of the liquid to form a gaseous O2/N2O mixture.
Critical & Pseudocritical temperature
The critical temperature of a gas is the maximum temperature at which compression can cause liquefaction. Or it is the temperature above which a substance cannot be liquefied however much pressure is applied. Mixing gases may change their critical temperature.
The pseudocritical temperature applies to a mixture of gases, such as Entonox, and is the temperature at which gas mixtures separate into their component parts.
The Poynting effect produces a 50:50 mixture which reduces the crtical temperature of N20 so Entonox has a pseudocritical temperature of -6 degree.
Entonox
Highest -5.5°C @117 bar
Cylinder -7°C @137 bar
Pipeline -30°C @4 bar
In cylinders it is supplied at a pressure of 137 bar and must be stored above its pseudocritical temperature of -6°C.
Below this temperature the N2O liquefies in a process called lamination. If this occurs a high concentration of O2 will be delivered first with little analgesic effect, but as the cylinder empties the mixture will become progressively more potent and hypoxic as it approaches 100% N2O.
If a cylinder has been exposed to cold below -6 degree C it should be warmed for 5 minutes in a 37 degree C water bath or for 2 hours in a room at 15 degree C. It should then be inverted three times before use.
When delivered via a pipeline at 4.1 bar the pseudocritical temperature is less than -30°C.
Altitude per se has no effect on Entonox.
Reference: www.frca.uk