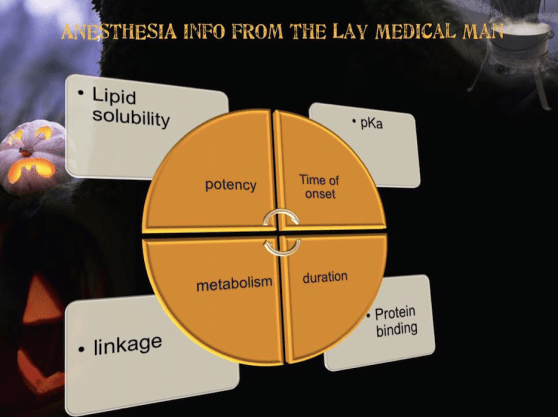
POTENCY:
Is affected by several factors including:
Hydrogen ion balance
Fiber size, type, and myelination
Vasodilator/vasoconstrictor properties (affects rate of vascular uptake)
Frequency of nerve stimulation
pH (acidic environment will antagonize the block)
Electrolyte concentrations (hypokalemia and hypercalcemia antagonizes blockade)
Lipid solubility.
DURATION OF ACTION
Is associated with lipid solubility.
Highly lipid soluble local anesthetics have a longer duration of action due to decreased clearance by localized blood flow and increased protein binding.
ONSET OF ACTION
Local anesthetics are weak bases and contain a higher ratio of ionized medication compared to non- ionized.
Increasing the concentration of non-ionized local anesthetic will speed onset.
In general, local anesthetics with a pKa that approximates physiologic pH have a higher concentration of non- ionized base resulting in a faster onset.
On the other hand, a local anesthetic with a pKa that is different from physiologic pH will have more ionized medication which slows onset.
For example, the pKa for lidocaine is 7.8 and 8.1 for bupivacaine. Lidocaine is closer to physiologic pH than bupivacaine. Lidocaine has a greater concentration on non-ionized local anesthetic than bupivacaine which results in a faster onset.
Non-ionized and ionized portions of local anesthetic solution exert distinct actions.
Lipid soluble, non-ionized form of the local anesthetic penetrates the neural sheath and membrane.
In the cell, the non-ionized and ionized forms equilibrate.
The ionized form of the local anesthetic binds with the sodium channel. Once “bound” to the sodium channel, impulses are not propagated along the nerve.
Clinically, onset of action is not the same for all local anesthetics with the same pKa. This is due to the intrinsic ability of the local anesthetic to diffuse through connective tissue.
So in general, local anesthetics with a pKa closest to the physiological pH generally have a higher concentration of non-ionized molecules and a more rapid onset.
Two notable exceptions are chloroprocaine and benzocaine. Chloroprocaine has a high pKa and rapid onset. Benzocaine does not exist in an ionized form and exerts its effects by alternate mechanisms.