- The resting position of the lungs and chest wall occurs at FRC.
- If isolated, the lungs, being elastic, would collapse to a volume <FRC.
- The isolated thoracic cage would normally have a volume >FRC.
- Since the chest wall is coupled to the lung surface by the thin layer of intrapleural fluid between parietal and visceral pleura, opposing lung and chest wall recoil forces are in equilibrium at FRC.
- This produces a pressure of about −0.3 kPa [−2 mmHg ] in the pleural space.
- Normal inspiration reduces intrapleural pressure further to −1.0 kPa [−6 mmHg] but with forced inspiration it can reach negative pressures of −4.0 kPa or more.
- Intrapleural pressure may be measured by an intrapleural catheter or from a balloon catheter placed in the mid-oesophagus [Oesophageal pressures
tend to reflect intrapleural pressures] - In the upright adult the intrapleural pressure at the base of the lung is approximately 0.7 kPa greater than the pressure at the apex
- It will increase during coughing
- -1.0 kPa intrapleural pressure is equivalent to a distending transpulmonary pressure of +1.0 kPa
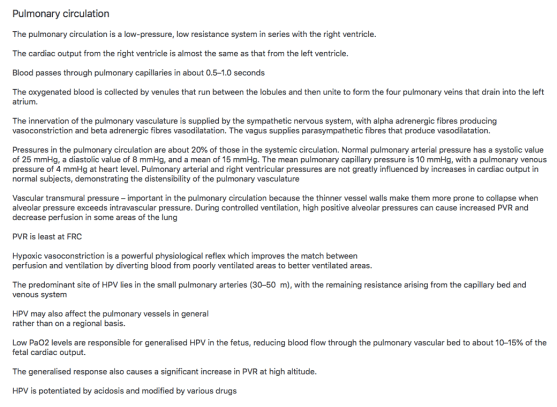
PULMONARY CIRCULATION
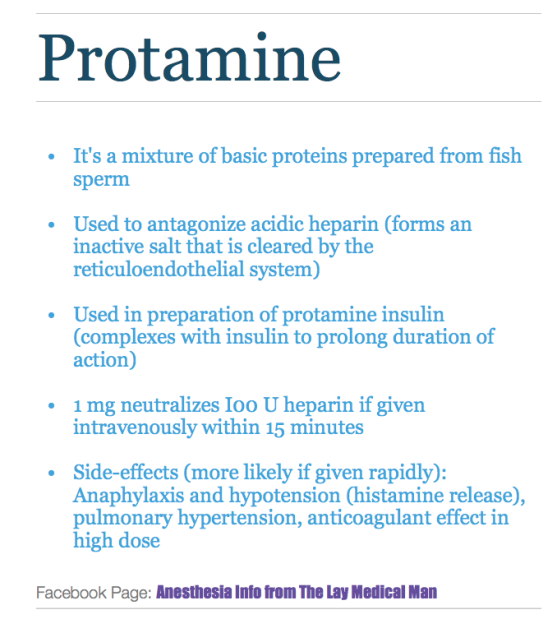
Protamine
DOXAPRAM

HOW DO YOU V😤MIT ❓

Management options in hypercalcemia
- Administration of normal saline
- Loop diuretics like Frusemide ( Thiazides will increase the tubular absorption of calcium)
- Calcitonin
- Bisphosphonates
- Mithramycin
- Hydrocortisone
- Hemodialysis
- Hypercalcemia per se doesn’t contraindicate any specific anesthetic drug or technique

TRANSFORMATION OF A PREGNANT LADY❗️ (When does the physiological changes of pregnancy comes back to normal?)
↪️Despite decreased requirements during pregnancy ,spinal anesthesia requirements return to non pregnant levels by 12-36 hours postpartum. Abouleish et al found that patients required 30% more bupivacaine, to achieve a T4 level for post partum tubal ligation , upto 24 hours after delivery. Rapid decline in plasma progesterone levels, after delivery of placenta is one factor, which contributes to this.
↪️Cardiac output rises immediately after delivery because of autotransfusion of 500 to 750 ml of blood from the uterus. Patients with pulmonary hypertension and stenotic valvular lesions are at a particular risk at this time.
↪️Cardiac output returns to slightly above prepregnancy values about 2 to 4 weeks after delivery.
↪️FRC and residual volume rapidly return to normal.
↪️Many of the pulmonary changes caused by mechanical compression by the gravid uterus resolve quickly. Alveolar ventilation returns to baseline by 4 weeks postpartum, and there is a rise in maternal PCO 2 as the progesterone levels decrease.
↪️The dilutional anemia of pregnancy resolves, and the hematocrit returns to normal within 4 weeks secondary to a postpartum diuresis.
↪️Serum creatinine, glomerular filtration rate, and BUN return to normal levels in less than 3 weeks.
↪️Mechanical effects of the gravid uterus on the gastrointestinal system resolve about 2 to 3 days after delivery; however, gastric emptying may be delayed for several weeks as serum progesterone levels slowly decrease.
#TubalLigation ,#pps , #PostpartumSterilization , #ObstetricAnesthesia , #ObstetricAnaesthesia, #PregnancyPhysiology ,#anesthesia , #anaesthesia ,#obstetrics , #pregnancy , #sterilization
Reference:
Shnider and Levinson's anesthesia for obstetrics, Maya Suresh; Sol M Shnider; Gershon Levinson, 2013,English : 5th
Ana M. Lobo, Andrea J. Fuller,Marina Shindell, Chapter 59, Anesthesia Secrets, 4/e
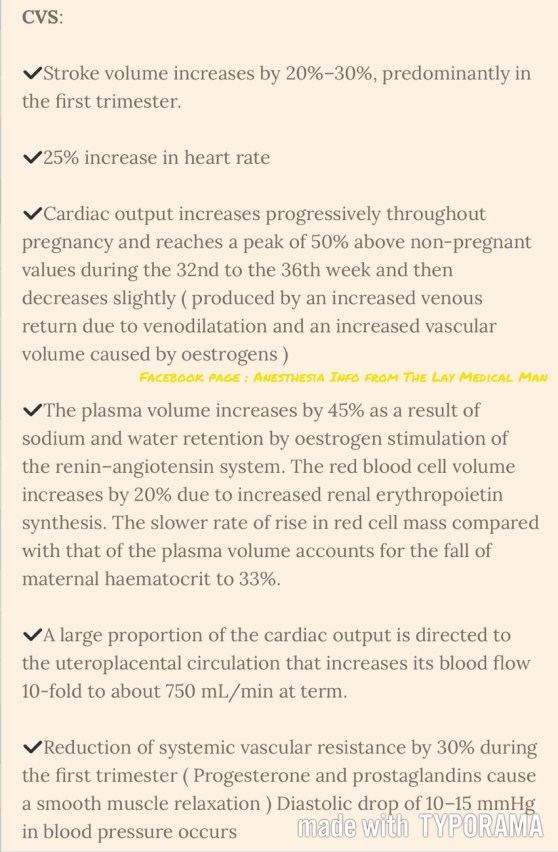
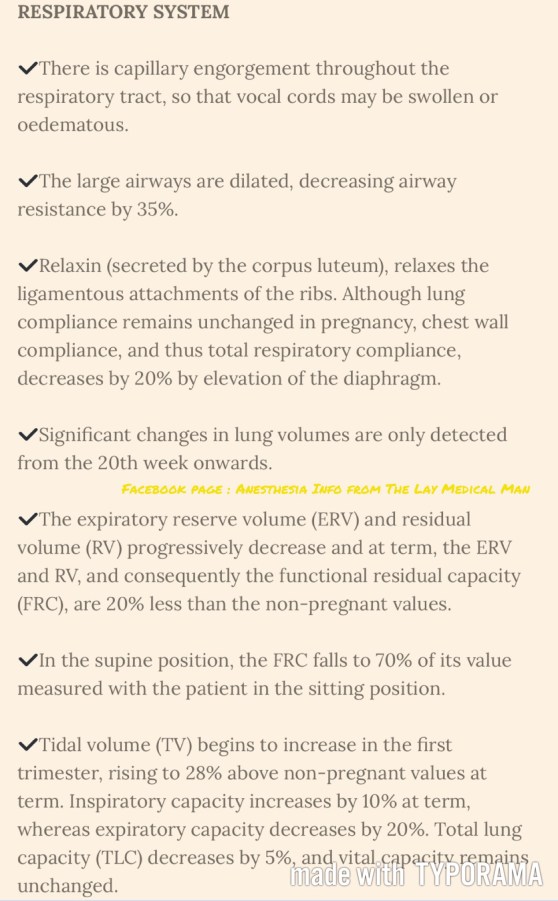
PREGNANCY: SUMMARY OF PHYSIOLOGICAL CHANGES



Ⓜ️NEMO #ANESTHESIA IMPLICATIONS IN SARCOIDOSIS: “SARC” 🔸🔸🔸🔸
🔻'S ound box(=larynx)' involvement
🔻Arrhythmia, Altered PFT-ECG-ECHO are key points to be searched for
🔻R enal impairement
🔻C alcium increased , Cardiac & CNS involvement
▪️ADDITIONAL POINTS▪️
PULMONARY INVOLVEMENT
➖➖➖➖➖➖➖➖➖➖
🔑PFT may be impaired
🔑CXR may show bilateral hilar lymphadenopathy with increased reticular shadowing in the lung fields
🔑Look for evidence of pulmonary hypertension
🔑If there is widespread pulmonary involvement and the patient is symptomatic, lung function tests, including blood gases, should be performed.
HYPERCALCEMIA
➖➖➖➖➖➖
🔑It is secondary to the production of excess 1,25- dihydroxycholecalciferol. Nephrocalcinosis and renal failure may occur . So establish treatment for hypercalcemia
CARDIAC INVOLVEMENT
➖➖➖➖➖➖➖➖➖
🔑Cardiac involvement carries a poor prognosis and it's diagnosis is of anaesthetic importance. Cardiac disease may be unexpected, and can occur even in young, previously asymptomatic patients.
🔑The pathological lesions can be diffuse or focal. Localised granulomas and fibrous scarring most commonly occur in the basal portion of the ventricular septum and left ventricular wall. These lesions will be asymptomatic unless they happen to involve the conducting system,in which case arrhythmias or conduction defects occur. Less commonly,the distribution of granulomas may be widespread,and they may coalesce to produce diffuse interstitial fibrosis. The resulting hypokinesia and subsequent heart failure is clinically indistinguishable from other cardiomyopathies .
🔑Pericardial effusions may also occur.Myocardial imaging showed that the majority of these had an infiltrative cardiomyopathy.
🔑In those patients diagnosed as having cardiac involvement,the signs in order of frequency of presentation were:
🔹complete heart block
🔹ventricular ectopics or ventricular tachycardia
🔹myocardial disease causing heart failure
🔹sudden death
🔹first-degree heart block or bundle branch block.
🔑In most of the patients with complete heart block and sarcoid the heart block was the first sign of the disease
🔑The sudden onset of complete heart block during anaesthesia can occur
🔑Difficulties with pacemaker management can be a feature of cardiac sarcoidosis. Patients with advanced disease may have automatic implantable cardioverter defibrillators inserted
🔑A preoperative ECG is essential, even in young patients. An ECHO also may be ordered. If there is evidence of a conduction defect, a temporary pacemaker should be inserted before anaesthesia.
CNS INVOLVEMENT
➖➖➖➖➖➖➖
🔑 Central nervous system sarcoid also carries a poor prognosis.
🔑 Presentation can vary widely and includes cranial nerve palsies,peripheral neuropathy,epilepsy,and cerebellar ataxia
AIRWAY INVOLVEMENT
➖➖➖➖➖➖➖➖
🔑 Laryngeal sarcoidosis : the commonest lesion reported is an oedematous, pale,diffuse enlargement of the supraglottic structures
🔑 Infiltration of the airway may cause obstructive sleep apnoea
🔑 So need for an ENT evaluation preoperatively should be considered
DIAGNOSIS :
➖➖➖➖
🔑 can be made on biopsy of a skin lesion,or lung and bronchial biopsy via a fibreoptic bronchoscope.
🔑 The Kveim test has a high positivity in the active stages, but is lower in the chronic disease.
🔑 Serum angiotensin- converting enzyme (ACE) level is an indicator of sarcoid activity
🔑 serum calcium and 24-h urinary calcium levels may also be increased in active sarcoid.
🔑 Treatment of active disease may include corticosteroids, immunosuppressants, methotrexate,NSAIDS,and calcium chelating agents.
Reference: Medical disorders and anaesthetic problems , Rosemary Mason , Anesthesia Databook , A Perioperative and Peripartum Manual , 3/e
#sarcoidosis , #mnemonics , #MedicalMnemonics , #anaesthesia
RESPIRATORY PHYSIOLOGY IN THE ELDERLY 👴🏻
🍃Ventilatory responses to hypoxia and hypercapnia are impaired secondary to reduced central nervous system activity.
🍃The respiratory depressant effects of benzodiazepines, opioids, and volatile anesthetics are exaggerated.
🍃These changes compromise the usual protective responses against hypoxemia after anesthesia and surgery in elderly patients.
🍃The loss of elastic recoil combined with altered surfactant production leads to an increase in lung compliance.
🍃Increased compliance leads to limited maximal expiratory flow and a decreased ventilatory response to exercise.
🍃Loss of elastic elements within the lung is associated with enlargement of the respiratory bronchioles and alveolar ducts, and a tendency for early collapse of the small airways on exhalation.
🍃There also is a progressive loss of alveolar surface area secondary to increases in size of the interalveolar pores of Kohn. This results in increased anatomic dead space, decreased diffusing capacity, and increased closing capacity all leading to impaired gas exchange.
🍃Loss of height and calcification of the vertebral column and rib cage lead to a typical barrel chest appearance with diaphragmatic flattening.
🍃The flattened diaphragm is mechanically less efficient, and function is impaired further by a significant loss of muscle mass associated with aging. Functionally, the chest wall becomes less compliant, and work of breathing is increased.
🍃Total lung capacity is relatively unchanged.
🍃Residual volume increases by 5% to 10% per decade.
🍃Vital capacity decreases.
🍃Closing capacity increases with age.
🍃Functional residual capacity (FRC) is determined by the balance between the inward recoil of the lungs and the outward recoil of the chest wall. FRC increases by 1%–3% per decade because at relaxed end expiration, the rate of decrease in lung recoil with aging exceeds that of the rate of increase in chest wall stiffness.
🍃In younger individuals, closing capacity is below functional residual capacity. At 44 years of age, closing capacity equals functional residual capacity in the supine position, and at 66 years of age, closing capacity equals functional residual capacity in the upright position.
🍃When closing capacity encroaches on tidal breathing, ventilation-perfusion mismatch occurs.
🍃When functional residual capacity is below closing capacity, shunt increases, and arterial oxygenation decreases. This results in impairment of preoxygenation. Increased closing capacity in concert with depletion of muscle mass causes a progressive decrease in forced expiratory volume in 1 second by 6% to 8% per decade.
🍃Increases in pulmonary vascular resistance and pulmonary arterial pressure occur with age and may be secondary to decreases in cross-sectional area of the pulmonary capillary bed. Hypoxic pulmonary vasoconstriction is blunted in elderly individuals and may cause difficulty with one-lung ventilation.
Ref: Geriatric Anesthesia 2/e , Miller’s Anesthesia 7/e
#Physiology , #Anesthesia , #Geriatrics
