CO2 ABSORBENTS
WHAT IS POYNTING EFFECT ❓
NEGATIVE PRESSURE PULMONARY OEDEMA
# NPPO is associated with upper airway obstruction in a spontaneously breathing patient.
# It occurs in 0.05–0.1% of all general anaesthetic cases and laryngospasm has been reported as being the cause in 50% of cases.
#The clinical course is most frequently observed on emergence from anaesthesia where incomplete recovery from general anaesthesia increases the likelihood of the development of laryngospasm, but it has also been reported after airway obstruction with a foreign body and blockage and biting of tracheal tubes, hanging, and strangulation.
#Pulmonary oedema is typically described as developing within 2 min of the obstruction.
Once the airway is occluded, the spontaneously breathing patient will continue to generate negative intrathoracic pressure which will increase substantially as respiratory distress develops.
#There is an associated increase in sympathetic tone due to the stress of hypoxia and airway obstruction which increases SVR and elevates pulmonary artery pressure.
This is further exacerbated by hypoxic pulmonary vasoconstriction.
#The combination of these processes creates a pressure gradient across the capillary–alveolar membrane which favours the movement of fluid into the lung parenchyma.
#It is most common in younger patients, presumably because they are able to generate higher negative inspiratory pressures and, arguably, have a higher sympathetic tone and better cardiac function.
#The condition may resolve rapidly after definitive management of the airway obstruction, but in some cases, copious pulmonary oedema may form and it can be associated with pulmonary haemorrhage suggesting capillary membrane damage.
#After recognition of the cause of obstruction, the treatment required ranges from relatively modest support such as brief periods of CPAP for 2 h to positive pressure ventilation over a period of 24 h.#TheLayMedicalMan
Ref: Neurogenic pulmonary edema, Ronan O’Leary, Justin McKinlay, Contin Educ Anaesth Crit Care Pain (2011) 11 (3): 87-92.
http://feeds.feedburner.com/TheLayMedicalMan
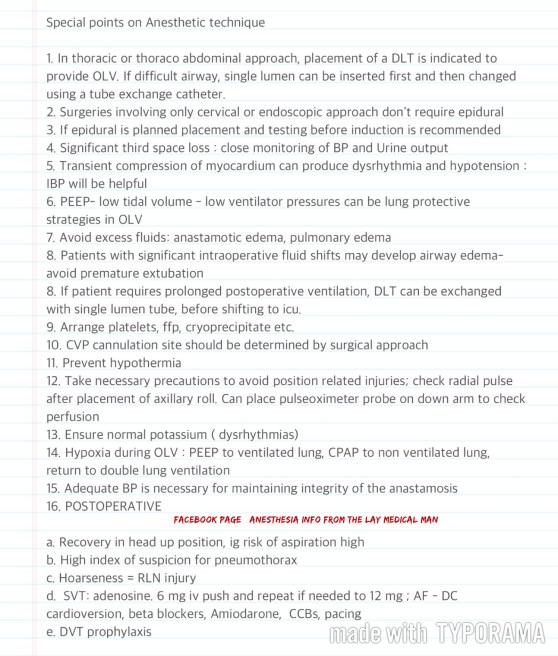
ANESTHESIA CONCERNS IN ESOPHAGEAL SURGERIES FOR MALIGNANCY
A FEW POINTS ABOUT A SHARED LUNG
🔸In the pregnant patient, the respiratory function deviates from the normal
🔸There is increased CO2 production by the mother and the foetus; but mostly you see a respiratory alkalosis. Why?
🔸This is because the stimuli from the raised pCO2 levels and that by the respiratory stimulant, progesterone, sets the minute ventilation approximately 30% higher than the normal levels and this is more than what is needed to compensate for the increased CO2 production
🔸It is mainly the reduction in FRC (a reduction by 10-25% ; appears by 12th week ; is due to the reduced chest wall compliance ; lung compliance is normal ) which makes the patient more vulnerable to hypoxia.
🔸The alveolar diffusing capacity is reported to be normal during pregnancy
#SCAVENGING IN #ANESTHESIA
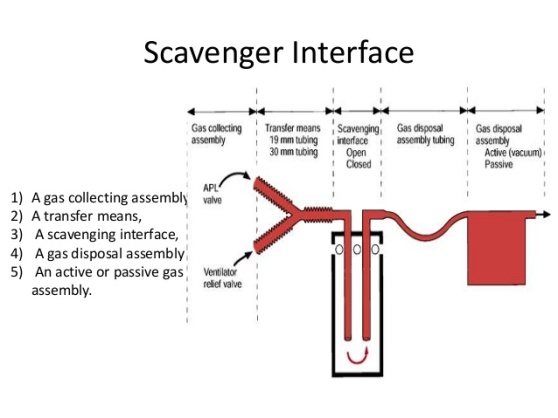 Scavenging refers to the method of extracting waste gases from the breathing system and venting them to an area where they will not be directly inhaled by staff or other patients.
Scavenging refers to the method of extracting waste gases from the breathing system and venting them to an area where they will not be directly inhaled by staff or other patients.
- Scavenging systems can be classified as open or closed.
- Open refers to the basic system of extracting the gas from its point of entry into the theatre
- Closed systems are more common and can be further subdivided into active and passive
- No conservation of volatile agent is possible with either the active or the passive systems; conservation must occur within the anaesthetic breathing system itself, by the use of a circle system and low-flow anaesthesia.
- The active and the passive both pass any waste gas to the atmosphere, polluting it to the same extent.
- In the passive scavenging system an exhaust port collects the waste gases from the expiratory valve of the breathing system or from the ventilator and the gases pass through the transfer system (which consists of 30 mm low-resistance tubing) to the outside of the building, preferably above roof level.
- If the theatre air is not recirculated, the waste gases can be piped to the exit port of the theatre ventilation system.
- In the passive system, the gases are pushed to the atmosphere solely by the expiratory power of the patient
- If the pathway to the atmosphere involves a vertical passage of gas, then the patient must overcome the atmospheric pressure required to push the gas over this distance; may be several floors of hospital! Means significant forces has to be overcome.
- The use of gases with higher density, like nitrous oxide, adverse atmospheric conditions like high winds etc, will further increase the forces required to expel waste gases; this can even affect the cardiopulmonary status of the patient.
BRIEF FUNCTIONAL ANATOMY OF THE BRAIN
✔️Precentral gyrus contains the primary motor cortex
✔️Premotor cortex lies immediately anterior to Primary motor cortex ( Brodmann’s area 6 on the lateral surface of the frontal lobe.)
✔️Premotor cortex is active in response to EXTERNAL visual or somatic sensory cues (e.g. reaching for an object in full view, or identifying an object by touch alone). Also has role in bilateral postural fixation (e.g. stabilization of the hips during walking).
✔️The supplementary motor area occupies a neighbouring part of Brodmann’s area 6 on the medial surface of the frontal lobe.
✔️The supplementary motor area seems to respond to INTERNAL cues, especially intentions to make voluntary movements (even if the movement is not carried out).
✔️Lesions of the supplementary motor cortex are associated with contralateral inability to initiate movements (akinesia).
✔️The inferior frontal gyrus of the dominant hemisphere (usually the left) contains the (Broca’s) motor speech area (Brodmann’s areas 44 and 45)
✔️The somatic sensory cortex, occupies the entire postcentral gyrus (Brodmann’s areas 3, 1 and 2, rostral to caudal).
✔️ Caudal to the somatosensory cortex is the sensory association cortex, which is divided into a superior and an inferior parietal lobule by an intraparietal sulcus.
✔️ The superior lobule is thought to be responsible for conscious awareness of the contralateral half of the body. Lesions of this part of the cortex may result in neglect of the contralateral side of the body.
✔️ The inferior lobule in the dominant (usually left) hemisphere is associated with language functions.
✔️ The cortex adjacent to the parieto-occipital sulcus and the calcarine sulcus, which lies on the medial surface of occipital lobe, constitutes the primary visual cortex (Brodmann’s area 17).
✔️ The superior surface of the temporal lobe contains the primary auditory cortex (Brodmann’s areas 41 and 42), responsible for the conscious perception of sound. Unilateral lesions of the primary auditory cortex will therefore cause partial deafness in both ears.
✔️ The auditory association cortex, known as Wernicke’s area corresponds to Brodmann’s area 22 in the dominant hemisphere. It allows for understanding of the spoken word, and connects with other language areas of the brain.
✔️ The temporal lobe curls inward to form the hippocampus which lies in the floor of the inferior horn of the lateral ventricle, and forms part of the limbic system. Its functions relate to short-term memory and the emotional aspects of behaviour.
✔️ Lying close to the anterior end of the hippocampus is the amygdala. Its a mass of subcortical grey matter that also forms part of the limbic system. It is associated with the conscious appreciation of smells.
✔️ The insula is one of the cortical centres for pain, and is also involved in involuntary activities such as the control of viscera by the autonomic nervous system.
✔️ The basal ganglia includes
• striatum (caudate nucleus, putamen of the lentiform nucleus and the nucleus accumbens)
• pallidum (globus pallidus of the lentiform nucleus)
• subthalamic nucleus
• compact part of the substantia nigra
✔️ Four basic circuits are known to occur from the cerebral cortex, through the basal ganglia and back to the cortex, by a direct or indirect route:
-a motor loop is concerned with learned movements;
-a cognitive loop with motor intentions;
-a limbic loop with emotional aspects of movement and
-an oculomotor loop with voluntary saccades.
✔️ Limbic system is composed of the the parahippocampal and cingulate gyri, the septal area, the hippocampal formation and the amygdala. Declarative memory (i.e. of new facts and events) may occur as modifications of synapses within the hippocampus.
✔️ Diencephalon comprises, from superior to inferior, the epithalamus, thalamus, subthalamus and hypothalamus.
✔️ The thalamus is the largest component of the diencephalon and is composed of numerous nuclei.
✔️ The epithalamus consists principally of the pineal gland that secretes melatonin and is involved with circadian rhythm and regulation of the onset of puberty and the habenular nuclei.
✔️ The subthalamus contains the subthalamic nucleus which connects to the globus pallidus and substantia nigra and is involved with the control of movement.
✔️ The hypothalamus has important connections with the limbic system, a controlling influence on autonomic nervous system activity and a role in neuroendocrine function.
✔️ The cerebellum coordinates movement by maintenance of equilibrium, posture and muscle tone at an unconscious level. Also concerned with muscular coordination, including trajectory, speed and force of movements.
✔️ The tectum (roof) of the midbrain is formed by four colliculi –the paired superior colliculi are associated with the visual system, and the inferior colliculi with the auditory system.
#FunctionalAnatomy, #NeuroAnatomy, #NeuroAnesthesia, #Neurosurgery ,#brain
Reference: The brain: functional divisions, Leo Donnelly, Neurosurgery, Neuroradiology & Neurocritical Care in Anaesthesia
BE SENSITIVE ENOUGH TO SENSE SSEP (SOMATO SENSORY EVOKED POTENTIAL)❗️❗️
SSEP reflect the ability of a specific neural pathway to conduct an electrical signal from the periphery to the cerebral cortex.
👉🏿THIS IS WHAT WE DO:
A skin surface electrode is placed near a major peripheral mixed function (motor and sensory) nerve ; median and ulnar nerves are usually stimulated at the wrist overlying the path of the respective nerves with 2 electrodes (needle or surface), separated by 2 cm, with the cathode proximal and the anode distal –> a square-wave electrical stimulus of 0.2 to 2ms is applied at a rate of 1 to 2Hz. –> The stimulus intensity is adjusted to produce minimal muscle contraction (usually 10 to 60mA) –> The resulting electrical potential is recorded at various points along the neural pathway from the peripheral nerve to the cerebral cortex.
👉🏿COMMON SITES OF STIMULATION:
🔻Upper extremity : median and ulnar nerves at the wrist.
🔻Lower extremity : the common peroneal nerve at the popliteal fossa and the posterior tibial nerve at the ankle.
🔻Less commonly the tongue, trigeminal nerve, and pudendal nerve have been studied.
👉🏿RECORDING:
After upper limb stimulation, potentials are recorded at the brachial plexus (Erb’s point, 2 cm superior to the clavicular head of the sternocleidomastoid muscle), the cervicomedullary junction (posterior midline of the neck at the second cervical vertebra), and the scalp overlying the somatosensory cortex on the contralateral side.
After stimulation of the lower extremity, potentials are recorded at the popliteal fossa, lumbar and cervical spinal cord, and somatosensory cortex. It is important to record nerve and subcortical potentials to verify adequate stimulation and delineate anesthetic effects.
👉🏿PLOTTING:
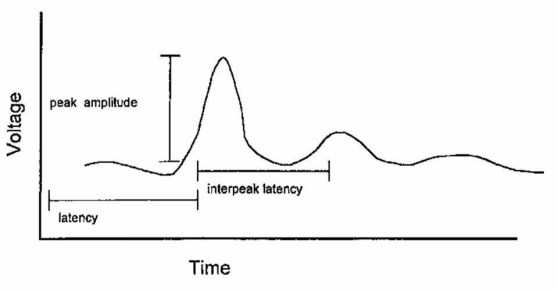
The SSEP is plotted as a waveform of voltage vs. time.
It is characterized by:
# Amplitude (A), which is measured in microvolts from baseline to peak or peak to peak
# Latency (L), which is the time, measured in milliseconds, from onset of stimulus to occurrence of a peak or the time from one peak to another
👉🏿MORPHOLOGY:
described as positive (P, below the baseline) or negative (N, above the baseline)
A waveform is identified by the letter describing its deflection above or below the baseline followed by a number indicating its latency (e.g., N20)
👉🏿INTRAOPERATIVE SSEP’s, INDICATIVE OF SURGICAL TRESSPASS / ISCHEMIA INCLUDE
a . increased latency
b . decreased amplitude
c . complete loss
Any decrease in amplitude greater than 50% or increase in latency greater than 10% may indicate a disruption of the sensory nerve pathways. The spinal cord can tolerate ischemia for about 20 minutes before SSEPs are lost.
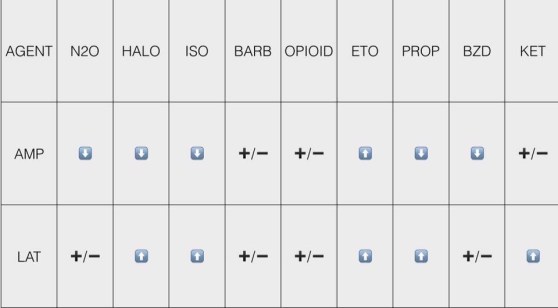
👉🏿ANESTHETIC DRUGS AND SSEP
All of the halogenated inhaled anesthetics probably cause roughly equivalent dose-dependent decreases in amplitude and increases in latency that are further worsened by the addition of 60% nitrous oxide. It is best to restrict the use of volatile anesthetics and nitrous oxide to levels below 1 minimum alveolar concentration (MAC) and not to combine the two. n If possible, bolus injections of drugs should be avoided, especially during critical stages of the surgery. Continuous infusions are preferable.
👉🏿CONDITIONS ALTERING SSEP
# Hypothermia : increases latency, whereas amplitude is either decreased or unchanged. For each decrease of 1 degree C, latency is increased by 1ms.
# Hyperthermia (4 degree C) : decreases amplitude to 15% of the normothermic value.
# Hypotension: With a decrease of the mean arterial blood pressure (MAP < 40mm Hg), progressive decreases in amplitude are seen. The same change is also seen with a rapid decline in MAP to levels within the limits of cerebral autoregulation.
# Hypoxia: ?Decreased amplitude
# Hypocarbia: Increased latency has been described at an end-tidal CO 2 < 25mm Hg.
# Isovolumic hemodilution: Latency is not increased until the hematocrit is < 15%, and amplitude is not decreased until the hematocrit is < 7%. This effect is likely caused by tissue hypoxia.
👉🏿INTRAOPERATIVE USES
🔻scoliosis surgery & Harrington rod placement
🔻spinal cord decompression and stabilisation after acute SCI spinal fusion
🔻brachial plexus exploration following acute injury
🔻resection of spinal cord tumours, cysts & vascular anomalies
🔻correction of cervical spondylosis
🔻resection of 4 th ventricular cysts
🔻release of tethered spinal cord
🔻resection of acoustic neuroma
🔻resection of intracranial lesions involving the sensory cortex
🔻resection of thalamic tumours
🔻abdominal and thoracic aneurysm repair
👉🏿IF SSEP CHANGES SIGNIFICANTLY, WHAT THE SURGEON AND ANAESTHESIOLOGIST CAN DO TO DECREASE THE INSULT?
The anesthesiologist can:
🔻Increase mean arterial blood pressure, especially if induced hypotension is used.
🔻Correct anemia, if present.
🔻Correct hypovolemia, if present.
🔻Improve oxygen tension.
🔻Correct hypothermia, if present.
The surgeon can:
🔻Reduce excessive retractor pressure.
🔻Reduce surgical dissection in the affected area.
🔻Decrease Harrington rod distraction, if indicated.
🔻Check positioning of associated instrumentation (e.g., screws, hooks).
🌀If changes in the SSEPs persist despite corrective measures, a wake-up test may be performed to confirm or refute the SSEP findings. The patient’s anesthetic level is lightened, and a clinical assessment of neurologic function is performed. The monitoring of motor-evoked potentials along with SSEPs provides a more complete assessment of neural pathway integrity. As the sensory pathways are supplied predominantly from the posterior spinal artery & the motor tracts from the anterior, a significant motor deficit can develop without significant change in SSEP’s.
#ssep ,#neuroanaesthesia , #anaesthesia , #neuromonitoring , #evokedpotential
HOW EVOKED POTENTIALS BEHAVE , WHEN BRAIN SUFFERS FROM ISCHEMIA ❓
🕶Cerebral ischemia slows neurotransmission and neuronal energy metabolism, resulting in decreased amplitude and increased latency of specific peaks.
🕶For SSEPs, a 50% reduction in amplitude and/or a 10% increase in latency [changes in the central conduction times, namely, the interpeak latencies between the N14 and N20 peaks] of SSEP signals from the baseline are generally accepted to be a significant change
🕶A 50% reduction on SEP amplitude has been shown to occur when cerebral blood flow decreases below 14 mL/100 g/min
🕶MEP have less well-defined warning criteria as compared to SSEPs; however, increased stimulus thresholds and/or decreased MEP amplitudes in relation to dramatic events (i.e., clip application) are indicative of pending neurologic insult.
🕶For BAEP, an increase in latency of more than 1 msec, particularly in wave V, is considered to be clinically significant.
🕶Unlike #EEG monitoring the evoked potential tests can detect subcortical functional status by way of perforating branches such as the anterior choroidal and medial striate arteries
Reference: Anesthesiology Research and Practice Volume 2014, Article ID 595837, Controversies in the Anesthetic Management of Intraoperative Rupture of Intracranial Aneurysm, Tumul Chowdhury, Andrea Petropolis,Marshall Wilkinson, Bernhard Schaller Nora Sandu and Ronald B. Cappellani
#neuroanaesthesia , #neuroanesthesia , #EvokedPotential , #neurosurgery , #anesthesiologist , #anesthesia .