TBI MANAGEMENT (Based on BTF 4e Guidelines)
- Principal of management of head injury is to prevent secondary brain injury due to hypoxia, hyper/hypocarbia, hypovolaemia, hypotension, and increased ICP.
- Primary survey and management of other life-threatening injury (tension pneumothorax, cardiac tamponade, airway obstruction, etc.) assessment with GCS
- Continuous high-flow O2 for all potential TBI cases
- Airway repositioning maneuvers if needed
- Evaluate the GCS. GCS<8, increased risk of aspiration, concern for hypoxemia and hypercarbia, need for hyperventilation: all such concerns when present are addressed with intubation and mechanical ventilation.
- C-Spine imaging based on NEXUS or Canadian C Spine rule criteria (see below)
- Obtain large bore IV’s and/or central venous access for patients requiring vasoactive drugs. For surgical procedures:
- ASA monitors along with direct intra-arterial pressure monitoring (zeroed at the level of the head to facilitate assessment of cerebral perfusion pressure [CPP]) and bladder catheterization are established. Avoid hypotension due to induction drugs and surges in BP during intubation and pinning using slow drug administration and vasoactive drugs.
- All attempts at intubation should include in-line neck stabilization. Anesthetic drugs that allow for rapid control of the airway while avoiding an increase in intracranial pressure (ICP) and providing hemodynamic stability are preferred. For rapid sequence intubation, succinylcholine or rocuronium may be used.
- Choice of drugs must be tailored to each individual patient. IV anesthetics are cerebral vasoconstrictors whereas volatile agents increase cerebral blood flow (CBF) above 1 MAC
-
Lidocaine in doses of 1.5 mg/kg may inhibit the adverse effects of laryngoscopy decreasing ICP, CMR, and CBF with minimal hemodynamic effects
- Careful positioning to avoid impedance to venous drainage due to extreme neck rotation or tilt. Avoid ties around the neck for endotracheal tube fixation
- Avoid increases in intrathoracic pressure (obstructed endotracheal tubes, bronchospasm).
- Maintain SBP at ≥ 110 mmHg for patients 15 to 49 or over 70 years and at ≥ 100 mmHg for patients 50 to 69years old. The recommended target CPP value is between 60 and 70 mmHg
- Isotonic crystalloid is the preferred fluid..A single SBP measurement < 90 mmHg will initiate intravenous (IV) fluid resuscitation with an initial bolus of 1 L of NS/RL in adults and adolescents and 20 ml/kg in older children followed by maintenance rates to keep SBP ≥ 90 mmHg
- Also hypovolemia resulting from extracranial hemorrhage should be ruled out
- Maintain ETCO2 between 35 and 45 mmHg (4.5-6 kPa). Avoid hyperventilation, especially in the first 12 hours. If you are going to hyperventilate the patient, use jugular venous saturation monitoring to ensure the brain is getting enough oxygen
- ABGs to titrate the ventilation and manage the fluids and electrolytes administration and to decide on postoperative ventilation if needed
- Avoid hypo and hyperglycemia
- Anaesthetic technique should allow a smooth and rapid recovery and prompt neurological assessment. Again avoid bucking over the endotracheal tube. Labetalol can be used to control sympathetic surges during extubation
- Continuous monitoring to avoid hypovolemia, hypotension, hypercarbia, hypoxia, hypoglycemia and dyselectrolytemias post extubation
- Adequate perioperative analgesia is important to prevent further raise in ICP due to pain. Analgesic options: Paracetamol, opioids like fentanyl, scalp block
- Discuss with the neurosurgeon regarding expected neurological recovery and modify the decision for extubation accordingly
-
Propofol may be used for ICP control. High dose barbiturates are recommended to control ICP refractory to maximum standard surgical and medical treatments while ensuring hemodynamic stability
-
Drain CSF for the first 12 hours for patients with a GCS of less than 6. Continuous drainage is better than intermittent
-
ICP Monitoring is Indicated if GCS is 3-8 and an abnormal CT OR Indicated if GCS is 3-8, there is a normal CT, and any two of the following
- Age over 40
- Motor posturing
- Hypotension (SBP under 90 mmHg)
- GCS < 8 with ICP > 22 mmHg require intervention
-
Decompressive craniectomy has been used but has not been found to improve outcome
- Use routine protocol to prevent VAP; no need for prophylactic antibiotics
- “Stable” TBI should have TED stockings and heparin or clexane
- Osmotherapy may be used in herniating patients.
-
Treatment with anticonvulsants within 7 days of injury
-
Glucose-containing fluids should be avoided and blood sugar monitored to maintain levels between 4–8 mmol/L.
- INDICATIONS FOR CT SCAN: GCS < 13 on presentation • Suspected open or depressed skull fracture • Signs of basal skull fracture (haemotympanum, CSF leak from ear or nose, battle’s sign, panda eyes) • Focal neurological signs. Also: More than one episode of vomiting following head injury • History of loss of consciousness following injury or more than 30 minutes of retrograde amnesia of events immediately prior to injury • Mechanism of injury (e.g. cyclist or pedestrian struck by motor vehicle, occupant ejected from a motor vehicle)
- INDICATIONS FOR INTUBATION: GCS < 8 in adult and < 9 in paediatric patients • Seizure after trauma • Airway obstruction, airway injury • Severe facial injury (Le Fort fracture, mandible fracture) • Inability to maintain oxygenation/ventilation (PaO2 < 9 kPa on air or < 13 kPa with oxygen, PaCo2 < 4 kPa or > 6 kPa) • To facilitate transfer of patient to tertiary centre • Alcohol or other drug intoxication plus signs of head injury (Remember Brain–>Face–>Airway–>Lung–>Stomach!)
SHALL WE DO A C-SPINE IMAGING?
- Under the NEXUS guidelines, when an acute blunt force injury is present, a cervical spine is deemed to not need radiological imaging if all the following criteria are met:
- There is no posterior midline cervical tenderness
- There is no evidence of intoxication
- The patient is alert and oriented to person, place, time, and event
- There is no focal neurological deficit (see focal neurological signs)
- There are no painful distracting injuries (e.g., long bone fracture)
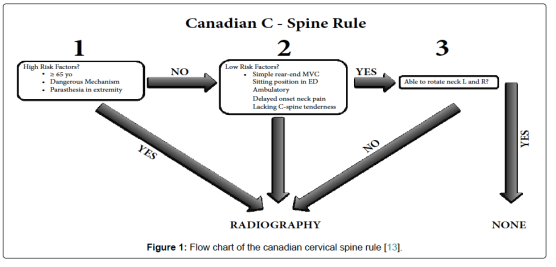
2. CANADIAN C-SPINE RULE
MANAGEMENT OF SDH: SPECIFIC POINTS
-
Subdural hematomas are the most common focal intracranial lesion
-
They have the highest mortality rate of all lesions , which is likely due to the associated brain injury and decrease in cerebral blood flow that accompany these lesions. Outcome worsens as the amount of midline shift exceeds the thickness of the hematoma
-
The hematoma is located between the brain and the dura and has a crescent shape. It is usually caused by tearing of the bridging veins connecting the cerebral cortex and dural sinuses
-
The management of these lesions is immediate surgical decompression, which has been shown to improve outcome
MANAGEMENT OF EDH: SPECIFIC POINTS
-
They generally have a better prognosis than subdural hematomas with the main determinant of outcome being preoperative neurologic status
-
Epidural hematomas are biconvex and are located between the dura and skull
-
The usual etiology is a torn middle meningeal artery, but the blood may also come from a skull fracture or bridging veins.
-
The classic presentation includes a lucid interval followed by neurologic deterioration and coma
-
Treatment is prompt surgical decompression when the following criteria are met: more than 30 mL for supratentorial and more than 10 mL for infratentorial hematomas, thickness of more than 15 mm, midline shift of more than 5 mm, or the presence of other intracranial lesions
-
Expectant management with close observation is acceptable for small lesions.
-
Since the brain parenchyma is usually not injured, the prognosis is excellent if the hematoma is rapidly decompressed

Good
LikeLike