| Bedside Test | Procedure | Normal / Reassuring Value | Clinical Significance (Red Flag) |
|---|---|---|---|
| Clinical Assessment | Observe for signs of respiratory distress and bulbar weakness (speech, swallowing). | No accessory muscle use, effortless breathing, strong cough, clear voice. | Tachypnea, accessory muscle use, paradoxical breathing, weak “boggy” cough, slurred/fading voice. |
| Vital Capacity (VC) | Patient takes a maximal inhalation and exhales fully into a bedside spirometer. | > 20 mL/kg (ideal body weight) | < 15-20 mL/kg, or a declining trend during the breathing trial. |
| Negative Inspiratory Force (NIF) / MIP | Patient makes a maximal inspiratory effort against an occluded airway for ~20 seconds. | More negative than -30 cm H₂O | Less negative than -30 cm H₂O (e.g., -25, -20), or a worsening trend. |
| Single Breath Count | Patient takes a deep breath and counts aloud steadily (e.g., “1-one-thousand, 2-one-thousand…”). | > 25 | < 15-20. Indicates severely reduced vital capacity. |
| Head Lift Test | Patient lies supine and lifts their head off the bed, holding the position as long as possible. | > 30 seconds | < 20 seconds. Correlates with significant diaphragmatic weakness. |
| Breath-Holding Time | After a maximal inhalation, the patient holds their breath for as long as possible. | > 30 seconds | < 20 seconds. Suggests poor respiratory reserve. |
Monthly Archives: August 2025
Pulsatility Index (PI)
The TCD Pulsatility Index (PI) is a parameter used in Transcranial Doppler (TCD) ultrasonography to evaluate the resistance to blood flow in cerebral vessels. It’s commonly used to assess cerebral hemodynamics, especially in patients with conditions like stroke, traumatic brain injury, hydrocephalus, and brain death.
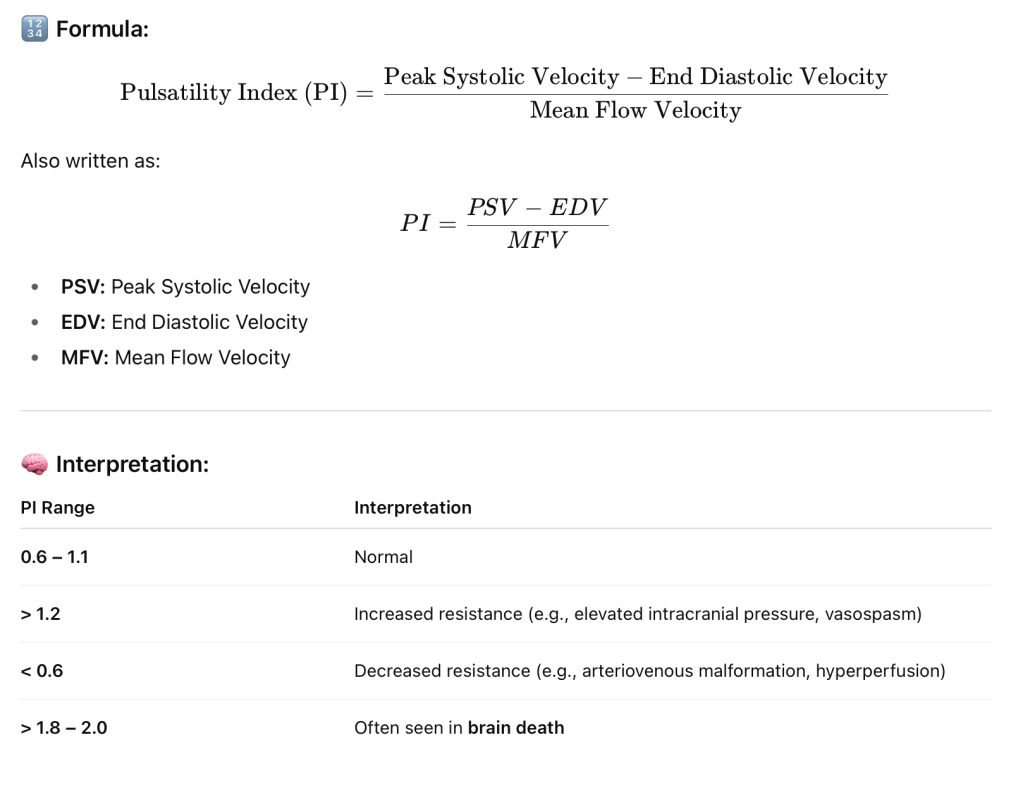
📌 Clinical Uses of PI in TCD:
- Elevated ICP (Intracranial Pressure): Higher PI suggests rising ICP.
- Vasospasm detection in subarachnoid hemorrhage.
- Brain death evaluation: Very high PI or absent diastolic flow.
- Monitoring cerebral autoregulation.
- Hydrocephalus assessment.
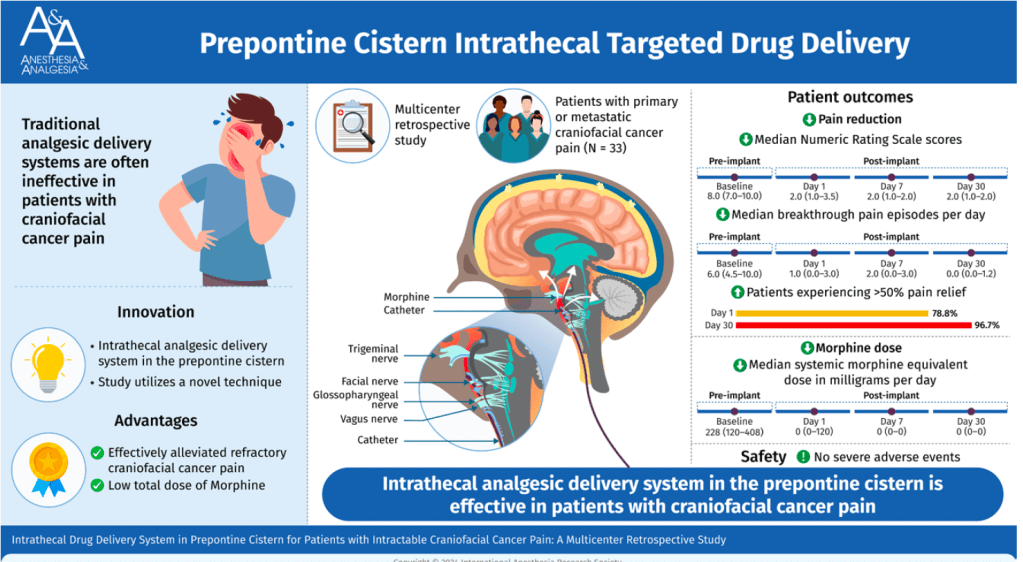
Intrathecal Drug Delivery System in Prepontine Cistern for Craniofacial Cancer Pain
Placing the catheter tip of an intrathecal morphine pump into the prepontine cistern could effectively relieve refractory craniofacial cancer pain with an extremely low total morphine dose requirement and few adverse events. This procedure could be considered in patients with severe refractory craniofacial cancer pain. (Anesth Analg 2025;141:255–63)
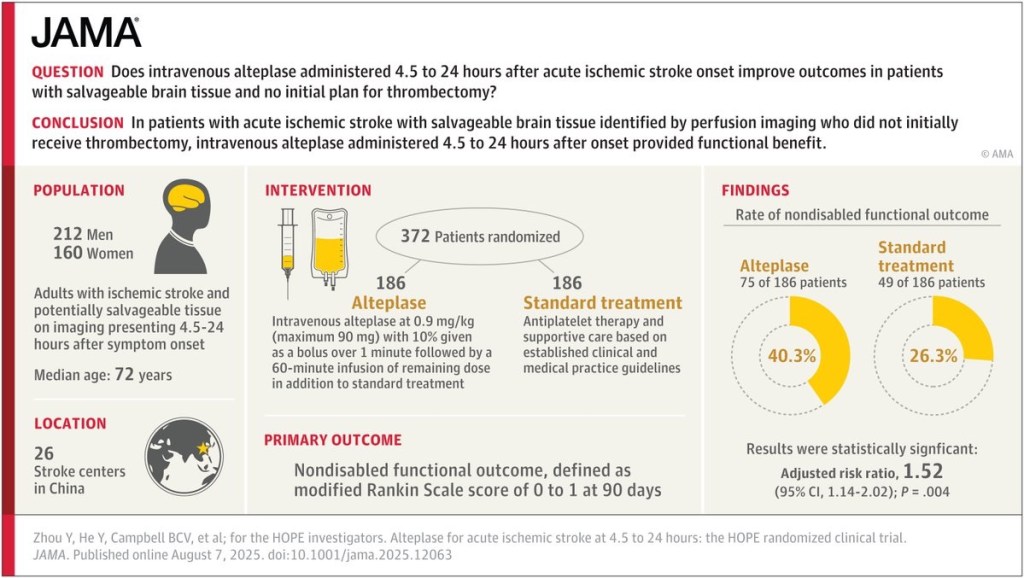
Does intravenous alteplase administered 4.5 to 24 hours after acute ischemic stroke onset improve outcomes?
Anaesthesia Machine Checklist
✅ ASA Summary of Anesthesia Machine Checkout Recommendations
🔄 To Be Completed Daily
1. Verify that auxiliary oxygen cylinder and self-inflating manual ventilation device are available and functioning
👥 Provider and Technician
2. Verify that patient suction is adequate to clear the airway
👥 Provider and Technician
3. Turn on anesthesia delivery system and confirm that AC power is available
👤 Provider or Technician
4. Verify availability of required monitors, including alarms
👤 Provider or Technician
5. Verify that pressure is adequate on the spare oxygen cylinder mounted on the anesthesia machine
👥 Provider and Technician
6. Verify that the piped gas pressures are ≥ 50 psig
👥 Provider and Technician
7. Verify that vaporizers are filled and, if applicable, filler ports are tightly closed
👤 Provider or Technician
8. Verify that there are no leaks in gas supply lines between flowmeters and common gas outlet
👤 Provider or Technician
9. Test scavenging system function
👤 Provider or Technician
10. Calibrate or verify calibration of the oxygen monitor, and check the low oxygen alarm
👤 Provider or Technician
11. Verify that carbon dioxide absorbent is not exhausted
👤 Provider or Technician
12. Perform breathing system pressure and leak testing
👥 Provider and Technician
13. Verify that gas flows properly through the breathing circuit during both inspiration and exhalation
👥 Provider and Technician
14. Document completion of checkout procedures
👥 Provider and Technician
15. Confirm ventilator settings and evaluate readiness to deliver anesthesia care (anesthesia time out)
👤 Provider
🕒 To Be Completed Prior to Each Procedure
2. Verify that patient suction is adequate to clear the airway
👥 Provider and Technician
4. Verify availability of required monitors, including alarms
👤 Provider or Technician
7. Verify that vaporizers are filled and filler ports are closed
👤 Provider
11. Verify that carbon dioxide absorbent is not exhausted
👤 Provider or Technician
12. Perform breathing system pressure and leak testing
👥 Provider and Technician
13. Verify gas flows properly through breathing circuit (inspiration and exhalation)
👥 Provider and Technician
14. Document completion of checkout procedures
👥 Provider and Technician
15. Confirm ventilator settings and evaluate readiness to deliver anesthesia care (anesthesia time out)
👤 Provider
Legend:
👥 = Provider and Technician
👤 = Provider or Technician / Provider only
