| Bedside Test | Procedure | Normal / Reassuring Value | Clinical Significance (Red Flag) |
|---|---|---|---|
| Clinical Assessment | Observe for signs of respiratory distress and bulbar weakness (speech, swallowing). | No accessory muscle use, effortless breathing, strong cough, clear voice. | Tachypnea, accessory muscle use, paradoxical breathing, weak “boggy” cough, slurred/fading voice. |
| Vital Capacity (VC) | Patient takes a maximal inhalation and exhales fully into a bedside spirometer. | > 20 mL/kg (ideal body weight) | < 15-20 mL/kg, or a declining trend during the breathing trial. |
| Negative Inspiratory Force (NIF) / MIP | Patient makes a maximal inspiratory effort against an occluded airway for ~20 seconds. | More negative than -30 cm H₂O | Less negative than -30 cm H₂O (e.g., -25, -20), or a worsening trend. |
| Single Breath Count | Patient takes a deep breath and counts aloud steadily (e.g., “1-one-thousand, 2-one-thousand…”). | > 25 | < 15-20. Indicates severely reduced vital capacity. |
| Head Lift Test | Patient lies supine and lifts their head off the bed, holding the position as long as possible. | > 30 seconds | < 20 seconds. Correlates with significant diaphragmatic weakness. |
| Breath-Holding Time | After a maximal inhalation, the patient holds their breath for as long as possible. | > 30 seconds | < 20 seconds. Suggests poor respiratory reserve. |
Author Archives: Dr Unnikrishnan Prathapadas
Pulsatility Index (PI)
The TCD Pulsatility Index (PI) is a parameter used in Transcranial Doppler (TCD) ultrasonography to evaluate the resistance to blood flow in cerebral vessels. It’s commonly used to assess cerebral hemodynamics, especially in patients with conditions like stroke, traumatic brain injury, hydrocephalus, and brain death.
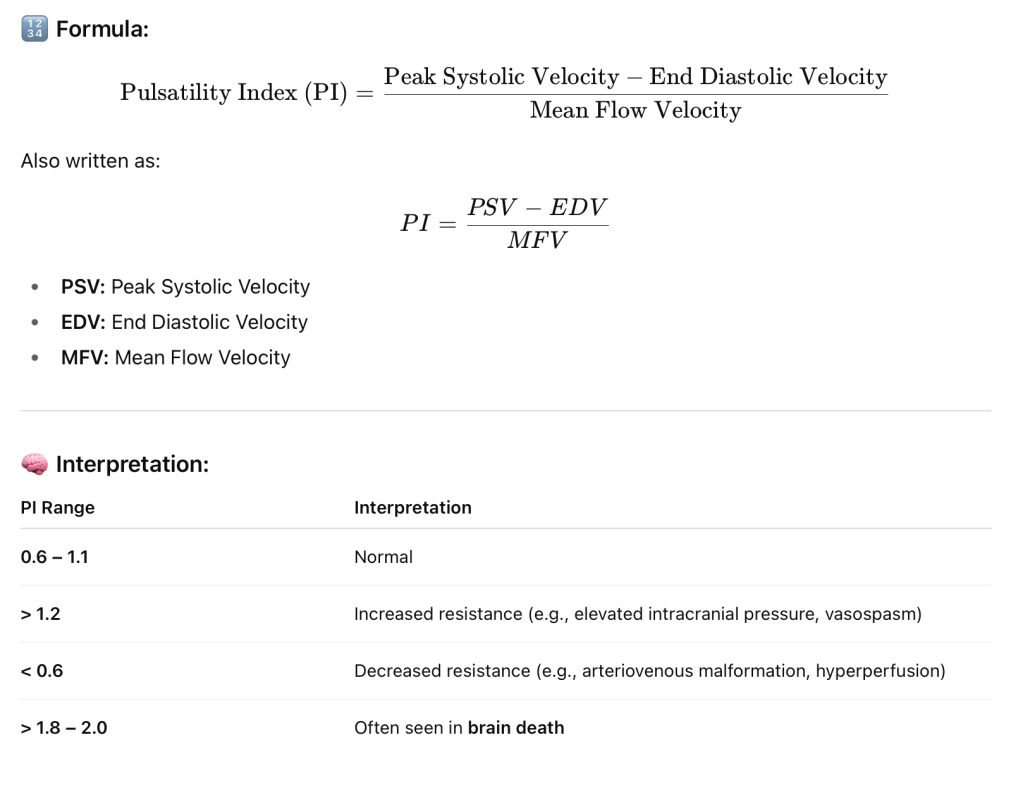
📌 Clinical Uses of PI in TCD:
- Elevated ICP (Intracranial Pressure): Higher PI suggests rising ICP.
- Vasospasm detection in subarachnoid hemorrhage.
- Brain death evaluation: Very high PI or absent diastolic flow.
- Monitoring cerebral autoregulation.
- Hydrocephalus assessment.
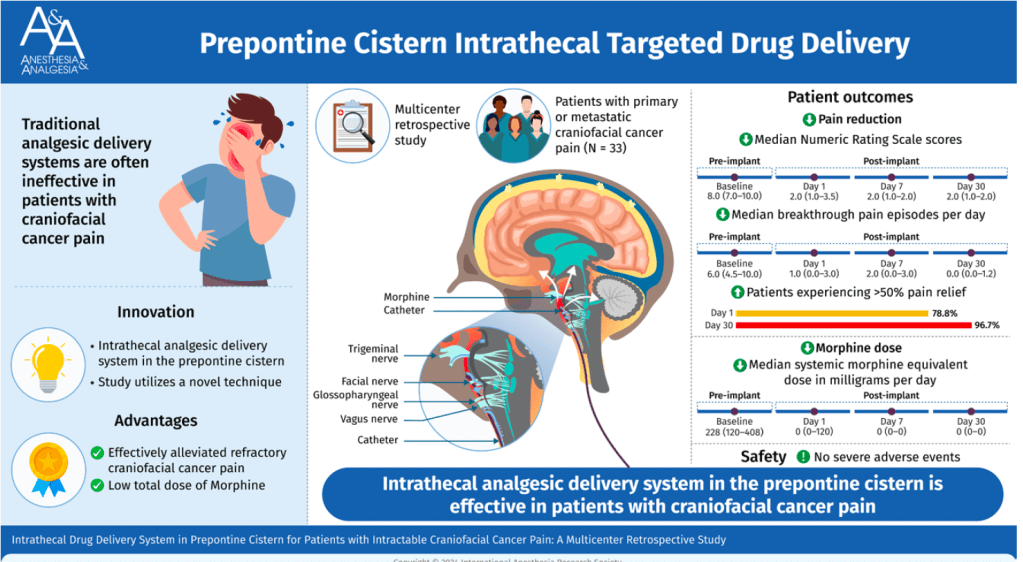
Intrathecal Drug Delivery System in Prepontine Cistern for Craniofacial Cancer Pain
Placing the catheter tip of an intrathecal morphine pump into the prepontine cistern could effectively relieve refractory craniofacial cancer pain with an extremely low total morphine dose requirement and few adverse events. This procedure could be considered in patients with severe refractory craniofacial cancer pain. (Anesth Analg 2025;141:255–63)
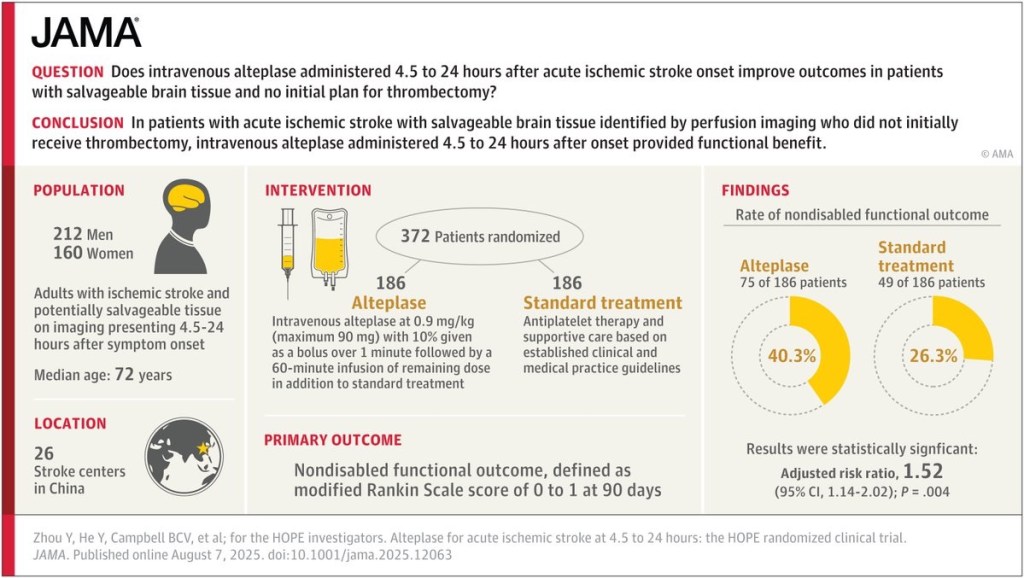
Does intravenous alteplase administered 4.5 to 24 hours after acute ischemic stroke onset improve outcomes?
Anaesthesia Machine Checklist
✅ ASA Summary of Anesthesia Machine Checkout Recommendations
🔄 To Be Completed Daily
1. Verify that auxiliary oxygen cylinder and self-inflating manual ventilation device are available and functioning
👥 Provider and Technician
2. Verify that patient suction is adequate to clear the airway
👥 Provider and Technician
3. Turn on anesthesia delivery system and confirm that AC power is available
👤 Provider or Technician
4. Verify availability of required monitors, including alarms
👤 Provider or Technician
5. Verify that pressure is adequate on the spare oxygen cylinder mounted on the anesthesia machine
👥 Provider and Technician
6. Verify that the piped gas pressures are ≥ 50 psig
👥 Provider and Technician
7. Verify that vaporizers are filled and, if applicable, filler ports are tightly closed
👤 Provider or Technician
8. Verify that there are no leaks in gas supply lines between flowmeters and common gas outlet
👤 Provider or Technician
9. Test scavenging system function
👤 Provider or Technician
10. Calibrate or verify calibration of the oxygen monitor, and check the low oxygen alarm
👤 Provider or Technician
11. Verify that carbon dioxide absorbent is not exhausted
👤 Provider or Technician
12. Perform breathing system pressure and leak testing
👥 Provider and Technician
13. Verify that gas flows properly through the breathing circuit during both inspiration and exhalation
👥 Provider and Technician
14. Document completion of checkout procedures
👥 Provider and Technician
15. Confirm ventilator settings and evaluate readiness to deliver anesthesia care (anesthesia time out)
👤 Provider
🕒 To Be Completed Prior to Each Procedure
2. Verify that patient suction is adequate to clear the airway
👥 Provider and Technician
4. Verify availability of required monitors, including alarms
👤 Provider or Technician
7. Verify that vaporizers are filled and filler ports are closed
👤 Provider
11. Verify that carbon dioxide absorbent is not exhausted
👤 Provider or Technician
12. Perform breathing system pressure and leak testing
👥 Provider and Technician
13. Verify gas flows properly through breathing circuit (inspiration and exhalation)
👥 Provider and Technician
14. Document completion of checkout procedures
👥 Provider and Technician
15. Confirm ventilator settings and evaluate readiness to deliver anesthesia care (anesthesia time out)
👤 Provider
Legend:
👥 = Provider and Technician
👤 = Provider or Technician / Provider only
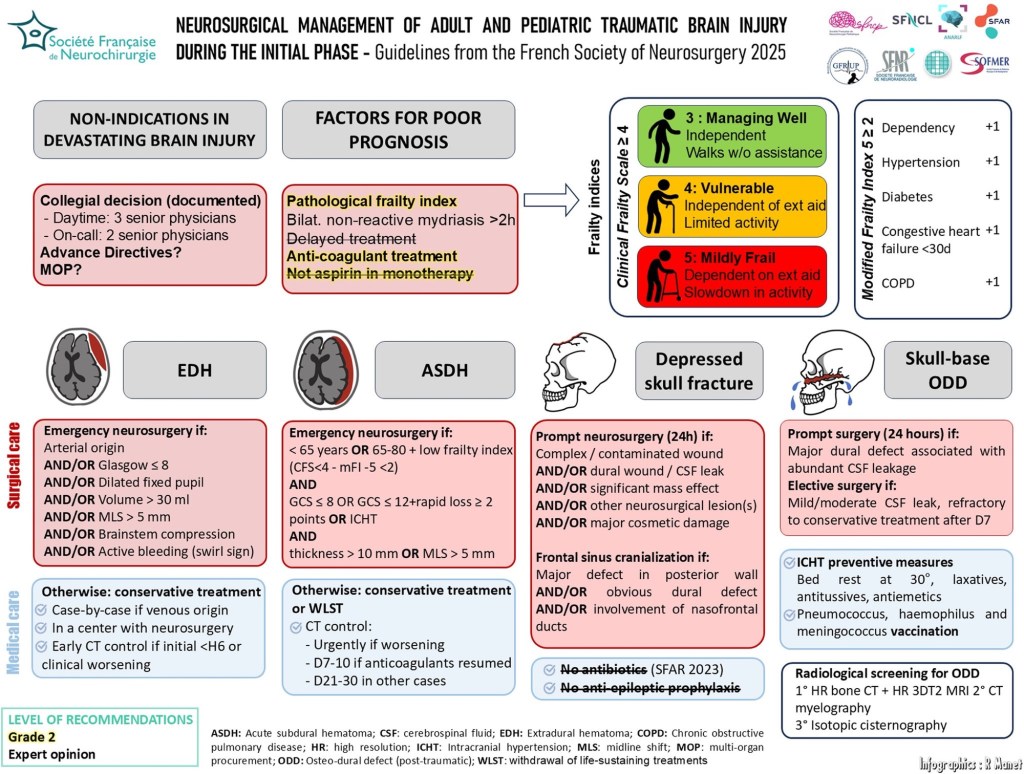
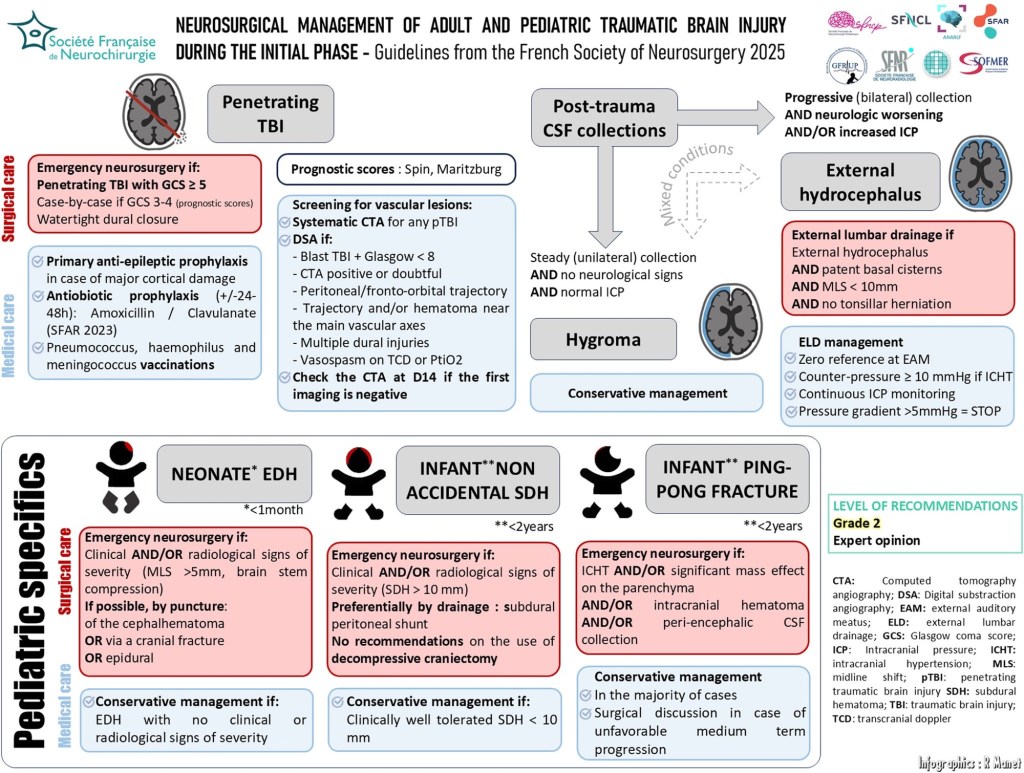
Neurosurgical management of the acute phase of adult and pediatric traumatic brain injury: 2025 guidelines of the French Society of Neurosurgery
Blood Transfusion in Pediatric Neurosurgeries: A Practical Guide
Introduction
Blood transfusion in pediatric neurosurgery, particularly for procedures like craniosynostosis repair, requires a careful and calculated approach. The unique physiological characteristics of children—especially infants—demand precise blood volume estimation, loss assessment, and transfusion decision-making to ensure safety and optimal outcomes.
Below are key calculations and considerations when planning for blood transfusion in pediatric neurosurgical settings:
1. Estimated Blood Volume (EBV)
Understanding the Estimated Blood Volume (EBV) is essential for predicting transfusion needs.
| Age Group | Estimated Blood Volume (ml/kg) |
|---|---|
| Preterm neonates | 90–100 |
| Full-term neonates | 85–90 |
| Infants (<12 months) | 80 |
| Children (>12 months) | 75 |
For example, in craniosynostosis surgeries, which often involve infants, use 80 ml/kg; for children like a 5-year-old patient, use 75 ml/kg.
2. Maximum Allowable Blood Loss (MABL)
To guide intraoperative transfusion decisions, MABL is calculated as:
MABL = EBV × (Starting Hct – Target Hct) / Starting Hct
This helps determine the volume of blood a child can safely lose before transfusion becomes necessary.
3. Packed Red Blood Cell (PRBC) Transfusion Volume
To avoid over-transfusion:
PRBC Volume (mL) = Weight (kg) × Desired Hb rise (gm/dL) × Transfusion Factor
Where:
- Transfusion Factor = 3 / PRBC Hct
(Typical PRBC Hct = 0.60–0.65)
Example: 10 mL/kg of PRBC with Hct 60% gives ~2 gm/dL rise in Hb.
4. Methods of Estimating Blood Loss
Estimating intraoperative blood loss in neurosurgery can be difficult due to hidden bleeding. Use a combination of the following:
- Visual assessment of the field
- Calibrated suction canister readings
- Weighing surgical sponges
- Serial haematocrit levels from ABG
- Thromboelastography (TEG) or ROTEM for coagulation monitoring
Note: Blood may be concealed under drapes or on instruments—constant vigilance is critical.
5. Factors Influencing Transfusion Decisions
There is no universal transfusion trigger; decisions must be individualized based on:
- Preoperative haematocrit and baseline haemoglobin
- Child’s weight and age
- Surgical pathology (e.g., craniosynostosis often involves blood loss >20–500% of EBV)
- Comorbidities affecting oxygen delivery (e.g., cyanotic heart disease)
Transfusion Thresholds and Recommendations
| Scenario | Transfusion Recommendation |
|---|---|
| Hb ≥ 7 gm/dL and stable | No transfusion needed |
| Hb < 5 gm/dL or critically ill | Transfusion indicated |
| Hb 5–7 gm/dL | Individualized decision |
| Target Hb after transfusion | 7.0 – 9.5 gm/dL |
| Minimum Hct for craniotomy | 25% |
| Optimum cerebral oxygen delivery | Hct ~30% |
| Acute brain injury (e.g., trauma) | Transfuse if Hb 7–10 gm/dL |
| Massive transfusion (>50% EBV in 3 hrs or 100% in 24 hrs) | Use PRBC : FFP : Platelet = 2 : 1 : 1 |
Summary
In pediatric neurosurgery, particularly in high-risk procedures like craniosynostosis repair, blood transfusion must be:
✅ Carefully calculated using weight-based formulas
✅ Guided by clinical condition, not just haemoglobin numbers
✅ Continuously reassessed using haematocrit, ABG, and coagulation studies
✅ Supported by a multidisciplinary team for timely intervention
By integrating these evidence-based parameters into your intraoperative workflow, you can significantly improve transfusion safety and patient outcomes.
Stay updated. Stay meticulous. Pediatric neurosurgery demands nothing less.
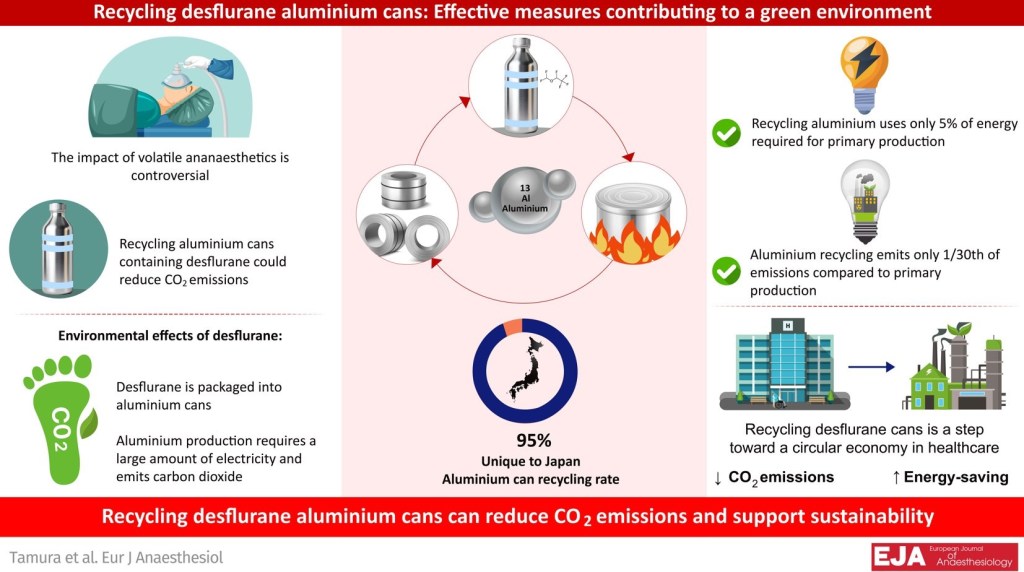
DESFLURANE CANS RECYCLING
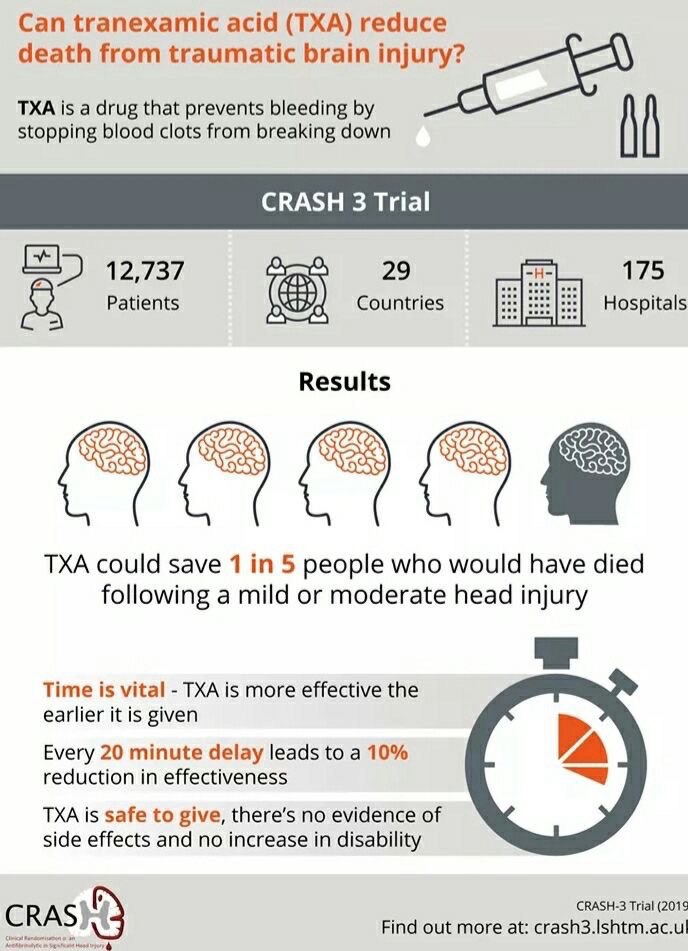
CRASH TRIAL
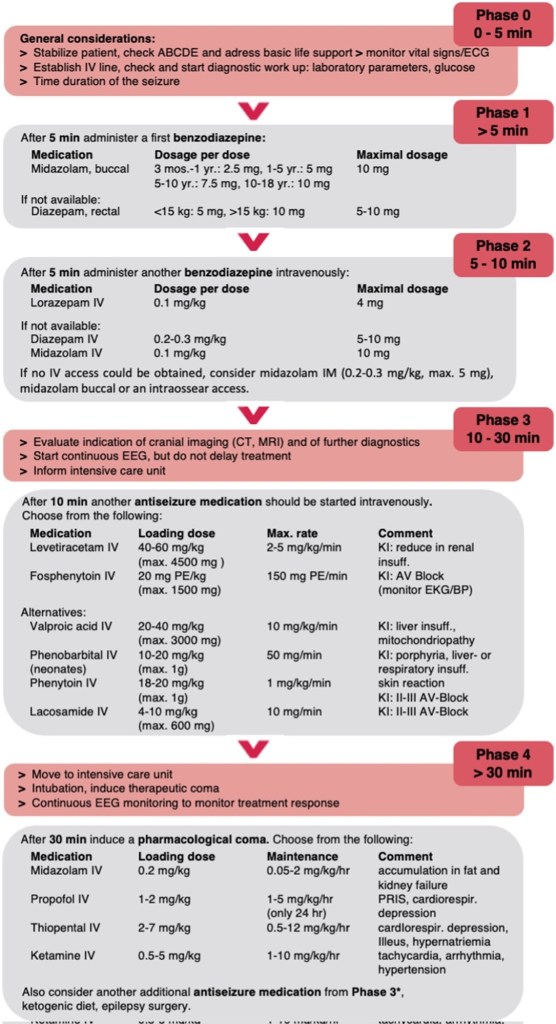
Pediatric Status Epilepticus Management