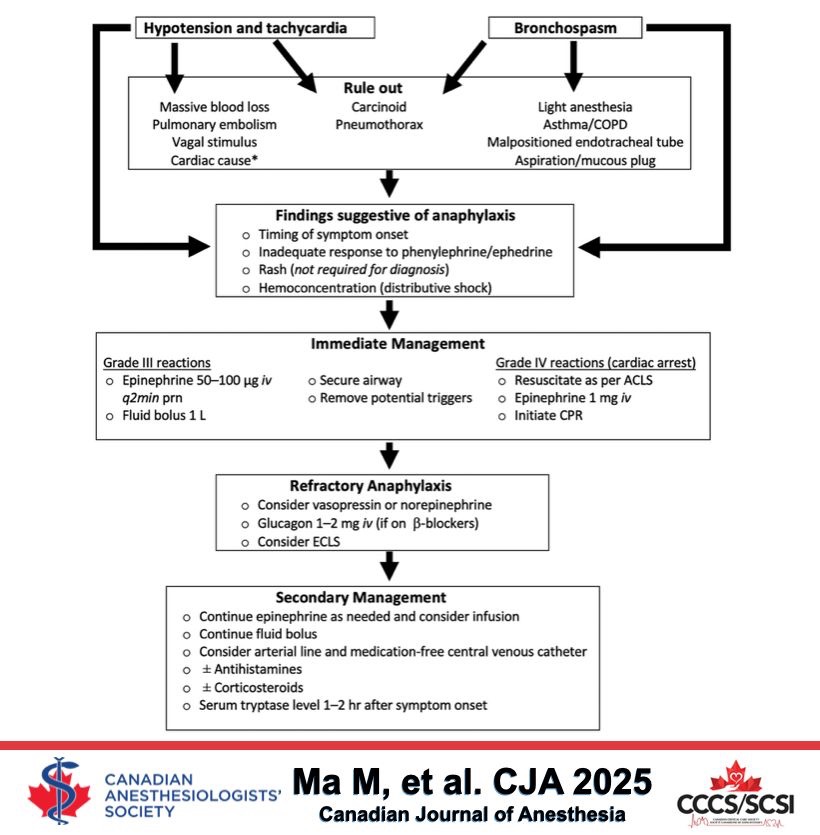
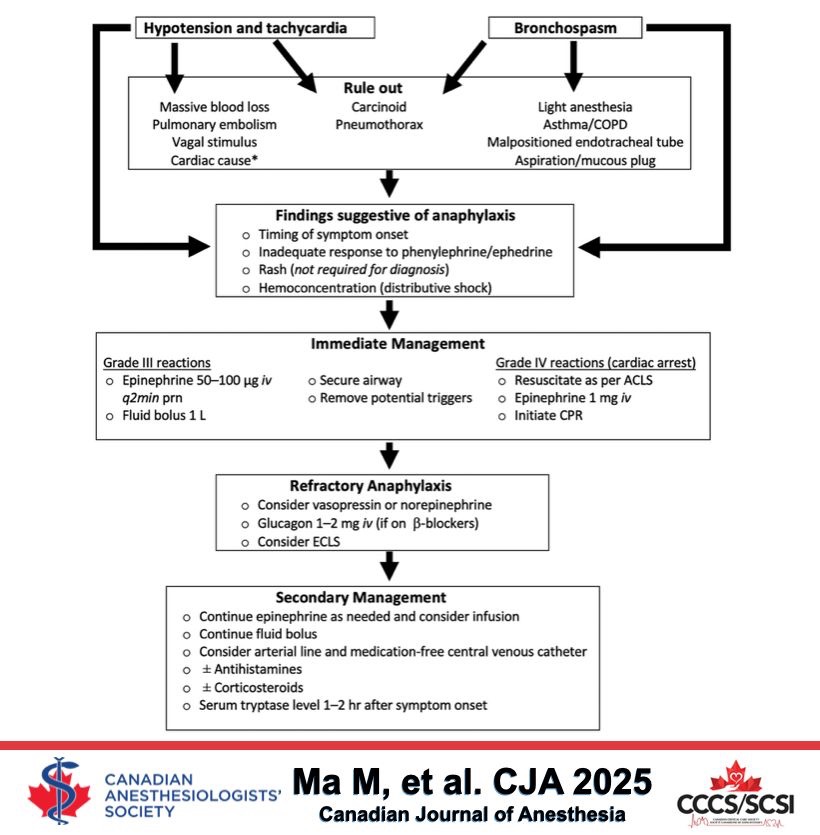
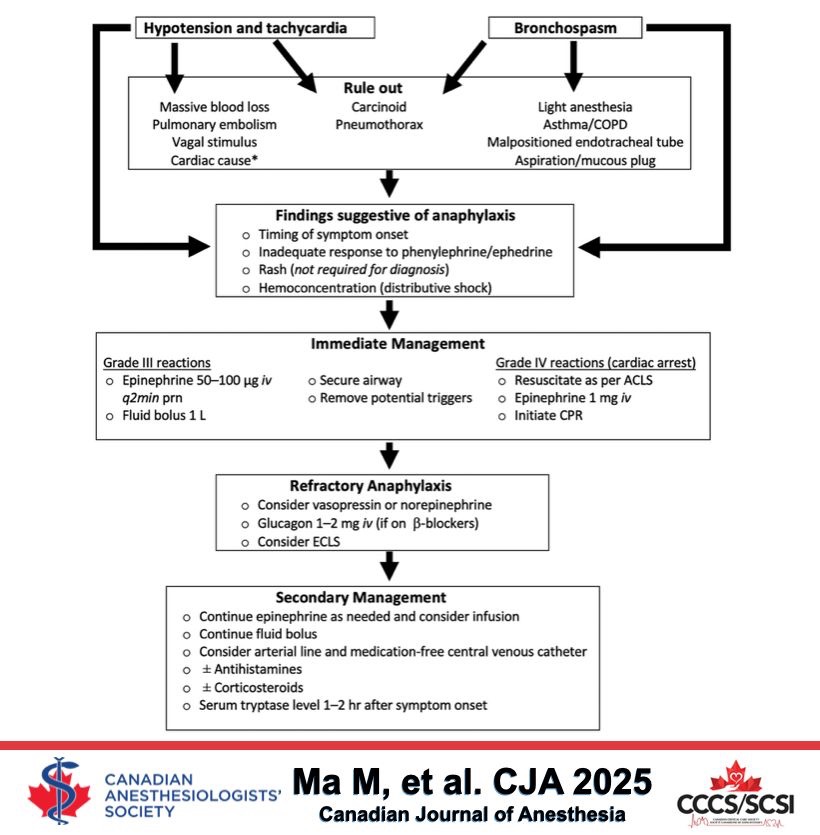
Perioperative Anaphylaxis


Corneal abrasion is the most common ocular complication after general anesthesia
Ischemic Optic neuropathy (ION) and Central Retinal Artery Occlusion (CRAO) are the commonest causes for postoperative visual loss
ISCHEMIC OPTIC NEUROPATHY (ION)
More common among the two
Most often seen after prolonged surgery in prone position
Venous congestion–> Raised Intra Ocular Pressure (IOP) due to Raised Intra Orbital Pressure –> Intra Orbital ‘Compartment Syndrome’
Hypotension, Diabetes, Vascular disease, Smoking etc also may be important in the etiopathogenesis
Treatment:
Reduce optic nerve edema as it passes through posterior scleral foramen with steroids and mannitol
Optimal oxygen delivery by ensuring normal blood pressure and hematocrit
Clear all obstruction to venous drainage
Chance of visual recovery is less
CENTRAL RETINAL ARTERY OCCLUSION (CRAO)
External pressure on eye and embolism are risk factors
An echocardiogram and carotid ultrasound may help us to find an embolic source
Reference: White E, David DB. Care of the eye during anaesthesia and intensive care. Anaesth Intens Care Med. 2007; 8(9): 383–386.
Neuromuscular blocking agents (NMBAs) represent the most frequently incriminated substances for allergic reactions among all drugs used in the perioperative period, ranging from 50 to 70% (1)
They are substances responsible for IgE-mediated anaphylaxis. Among NMBAs, the following substances have been incriminated, in decreasing order of importance: suxamethonium, vecuronium, atracurium, pancuronium, rocuronium, mivacurium and cisatracurium.(1)
Incidence of anaphylactic reactions are seen more with suxamethonium and rocuronium. (2) (3)
These reactions are more severe than with latex allergy
Seem to occur more frequently in women than in men.
If rapid-sequence induction is not mandatory, safer alternatives like cisatracurium can be used , in place of Rocuronium
Regarding suxamethonium, more frequently it causes histamine release from mast cells and basophils, resulting in flushing and urticaria (without anaphylactic reactions)(4)
Regarding atracurium , histamine release is observed in 40% of patients who receive doses over 0.5 mg/kg, resulting in transient hypotension and tachycardia; this can be prevented by injecting the drug slowly over 75 seconds, reducing the dose or prior treatment with 0.1 mg/kg chlorpheniramine and 2 mg/kg cimetidine i.v. (4)
Cisatracurium will not cause histamine release in clinical dose range. Cisatracurium had the lowest rate of cross-reactivity in patients who had previously suffered anaphylaxis to rocuronium or vecuronium.(4)
Mivacurium causes transient fall in b.p. due to histamine release with doses above 0.2 mg/kg(4)
The estimated sensitivity of skin tests for muscle relaxants is approximately 94 to 97 %. (1)
#anaphylaxis , #allergy , #anaesthesia , #MuscleRelaxants , #criticalcare , #nmba , #AnaesthesiaComplications , #pharmacology ,#rocuronium , #cisatracurium
Reference:
(1) www.worldallergy.org , Allergy to Anesthetic Agents, Mertes Paul Michel, Demoly Pascal, Stenger Rodolphe , Updated May 2013 ,Originally posted: October 2007, Reviewed by: Mario Sánchez-Borges
(2)A. Gullo(Editor) Anaesthesia, Pain, Intensive Care and Emergency – A.P.I.C.E.
(3) Proceedings of the 22 nd Postgraduate Course in Critical Care Medicine, Incidents Provoked Specifically by Certain Drugs Used in Anaesthesia M. K LIMEK , T.H. O TTENS ,F.G RÜNE
(4) Lee’s Synopsis of Anaesthesia,13/e, p:191-193
(5) Br J Anaesth. 2013 Jun;110(6):981-7. Anaphylaxis to neuromuscular blocking drugs: incidence and cross-reactivity in Western Australia from 2002 to 2011., Sadleir PH1, Clarke RC, Bunning DL, Platt PR.