>Sensitive to muscle relaxants
>Autonomic hyperreflexia , Avoid suxamethonium
>Bulbar palsy

>Sensitive to muscle relaxants
>Autonomic hyperreflexia , Avoid suxamethonium
>Bulbar palsy
Atropine produces complete vagal block at a dose of 3 mg;
Should be avoided in pyrexial children, as it inhibits sweating ;
Delirium is another side effect ;
Patients with Downs syndrome may show resistance to atropine;
Parenteral atropine wont cause significant pupillary dilatation and so is not contraindicated in glaucoma
Follow up the patient:
If voice is not improving: (Better to call the ENT Surgeon to do this-) Do a laryngoscopy and using any instrument, just give a mild pressure on aretynoid; usually it will fall back to correct position.
If speech is improving, advice VOCAL CORD ADDUCTION EXERCISES
Standing position.. Take a deep inspiration
and stop..and hold the breath.. this closes glottis..now strongly fall over and push against a wall…keep it for a few seconds.. Repeat this a few times.. This can force the aretynoid back to normal position by a stretching force… Usually voice is regained by this after 2 days..
Or lift heavy weights after deep inspiration (not for CAD patients)
Plus continue Speech Therapy
Problem occurs, when Aretynoid dislocates, and nobody attempts to relocate it, and it get fixed in that position..
INDICATIONS: 1. Diuretic (particularly in the presence of metabolic alkalosis) 2. Correction of severe metabolic alkalosis
DOSAGE: For diuresis, the dose is usually 250-375 mg stat. If, after an initial response, the patient fails to continue to diurese, do not increase the dose but allow for kidney recovery by skipping medication for a day. Acetazolamide yields best diuretic results when given on alternate days, or for 2 days alternating with a day of rest.Increasing the dose does not increase the diuresis and may increase the incidence of drowsiness and/or paraesthesia. Increasing the dose often results in a decrease in diuresis.
Evidence to support use in patients below the age of 12 years have not been established.
Acetazolamide is contraindicated in the presence of metabolic acidosis. This drug is not indicated in patients on renal replacement therapy.
Acetazolamide is an enzyme inhibitor that acts on carbonic anhydrase, the enzyme that catalyzes the reversible reaction involving the hydration of carbon dioxide and the dehydration of carbonic acid.
CONTRAINDICATIONS 1. Hypersensitivity to acetazolamide or other sulphonamides 2. Metabolic acidosis 3. Cirrhosis (risk of development of hepatic encephalopathy)
Acetazolamide and sodium bicarbonate used concurrently increases the risk of renal calculus formation.
METABOLIC SIDE EFFECTS
Metabolic acidosis, electrolyte imbalance, including hypokalaemia, hyponatraemia, loss of appetite, taste alteration, hyper/hypoglycaemia.
DO YOU KNOW?
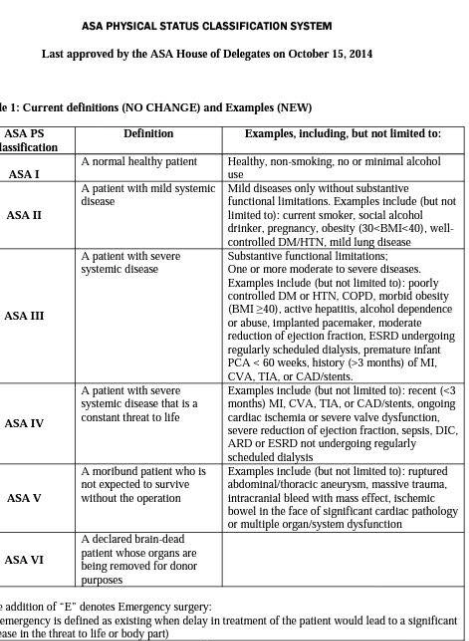
A social drinker is ASA II
A smoker is ASA II
Pregnant patient is ASA II
Obese patient is ASA II
Morbid obesity is not ASA II, but ASA III
Alcohol dependence without any documented systemic illness is also ASA III
Premature infant is ASA III
ESRD with regular HD is ASA III
ESRD without regular HD is ASA IV
Evidence of Sepsis or DIC- ASA IV
Intracranial bleed with mass effect is ASA V
A cardiac patient with bowel ischemia is ASA V
Continuous Intravenous Infusion
Magnesium sulfate 4-g to 6-g loading dose diluted in 100 mL fluid administered intravenously over 15 minutes, followed by continuous intravenous infusion at 1 to 2 g per hour. Discontinue 24 hours after delivery or last seizure.
If convulsions persist after 15 min, give up to 2 gram more intravenously as a 20% solution at a rate not to exceed 1g/min. If the patient weighs >70 kg then an additional 2 grams may be given slowly
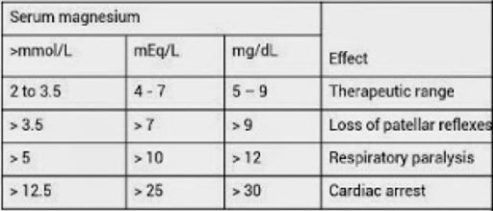
Only give the next IM dose, or only continue the IV infusion if:
Respiratory rate > 16/min
Urine output > 25 ml/h
Patellar reflexes are present
If urine output < 100 ml in 4 h and there are no other signs of magnesium toxicity, reduce the IV infusion to 0.5 g/h.
If patellar reflexes are depressed and respiration is normal, withhold further doses of magnesium sulfate until the reflexes return and request magnesium level.
If there is concern about respiratory depression , stop magnesium, give oxygen by mask and give:
Calcium gluconate (10mL of 10% solution over 10 minutes)
ACOG TASK FORCE 2013
… For women with severe preeclampsia, the administration of intrapartum and postpartum magnesium sulfate to prevent eclampsia is recommended. For women with preeclampsia undergoing cesarean delivery, the continued intraoperative administration of parenteral magnesium sulfate to prevent eclampsia is recommended.
ANESTHETIC CONCERNS
1. Short trachea with 15 rings or less; high chance of accidental one lung ventilation
2. Chances of Laryngeal Stenosis… Some times an unanticipated difficulty for passing tube, may trigger edema and stridor
3. Atlanto axial instability, can cause, massive cord edema, even with moderate neck flexion. Take LATERAL CERVICAL SPINE VIEWS IN FLEXION AND EXTENSION PREOPERATIVELY. If atlantoaxial instability is present and patient requires GA, give MANUAL IN LINE STABILIZATION/ do AWAKE FOB.
4. Restricted lung function accompanied by impending respiratory failure, is a situation, where we may be more inclined towards SAB in such patients (e.g. Pregnancy, where the uterus further compromise lung function). So regional anesthesia may be appropriate, if technically feasible.
5. Technical difficulties with SAB/EDB; epidural space located 2.5 cm from skin was reported in one case.
This is the most frequently occurring demyelinating neuromuscular disorder. It’s a chronic progressive disease characterized by repeated exacerbations and partial remissions. It is characterized by the formation of plaques within the brain and spinal cord. These plaques cause demyelination around the axons, resulting in weakness and spasticity as well as sensory dysfunction.Upper motor neurone lesions, cerebellar lesions and sensory deficits are common.
Anaesthetic considerations.
Regional blockade.
Temperature maintenance is important as symptoms can deteriorate with an increase in temperature, as demyelinated axons are also more sensitive to heat.
Most often, postop exacerbation, if it occurs, is due to fever and infections
We should explain the chance of exacerbation of symptoms before any form of regional anesthesia
TREATMENT
The treatment of MS includes treating acute attacks to limit sequelae, prophylactic medications to reduce rate of progression, and symptomatic/supportive therapy
Acute attacks are treated with high-dose corticosteroids, i.v. methylprednisolone 500–1000 mg every day divided every 6 or 12 hours; tapered over 7–10 days.
Prophylactic medications include the disease-modifying drugs interferon β and glatiramer acetate. Side effects include local infections, fatigue, depression, and anxiety. Regular CBC, LFT, and electrolyte checks are needed.
For progressive disease, immunomodulatory drugs such as methotrexate, cyclosporine, cyclophosphamide, azathioprine, total lymphoid irradiation, mitoxantrone (risk of cardiotoxicity), mycophenolate mofetil, or interferon-β may be employed
Symptomatic therapies include antidepressants for depression, anticholinergics for hyperreflexic bladder, alpha-blockers or cholinergics/catherization for flaccid bladder, amantadine for fatigue, antispasticity drugs (baclofen, tinzanidine, dantrolene, benzodiazepines) for muscle spasticity, AEDs for tremor, clonus, and pain, and sildenafil for sexual dysfunction. More invasive methods, for example, botulinum toxin injections for focal spasticity or bladder augmentation for spastic bladder may be required in more severe cases
Supportive care includes physical/occupational therapy, coping strategies or lifestyle modifications, cognitive-behavioral therapy, and emotional support.
In more severe cases, ambulatory aids or wheelchairs and other home-assist devices and caregiver support may be necessary
# Makes the RBC membrane friable and leads to episodic hemolytic anemia n jaundice
# Stress (surgery or anesthesia), drugs, newborn period, infection, exposure to fava beans are stimulants/risk factors.
# Culprit drug list is long: vit C n K, Methylene blue (caution in rx of methemoglobinemia),SNP, prilocaine.…
# Check for anemia, need for transfusion, jaundice(can also appear postop),cataract(increased incidence)
# Malignant Hyperthermia has been reported in association
# Avoid elective surgeries during a hemolytic episode
# Give a folic acid suppliment perioperatively
# Paracetamol,Phenytoin,L Dopa etc are safe.