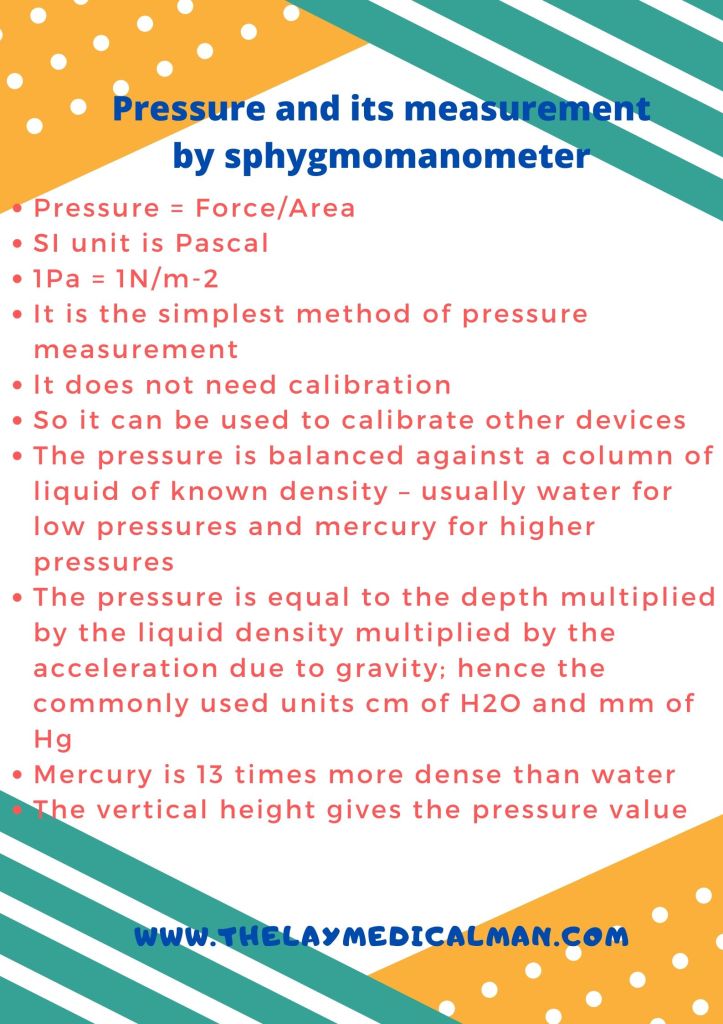
Pressure and it’s measurement by manometer


PREGANGLIONIC NEURONS of the sympathetic system synapse with the POSTGANGLIONIC NEURONS in the SYMPATHETIC GANGLIA. These ganglia together will form sympathetic chain. The sympathetic chains extend down the length of the vertebral column and are divided into four parts:
CERVICAL SYMPATHETIC GANGLIA
🔸Consist of three ganglia: Superior, Middle and Inferior
🔸Superior sends postganglionic fibres to form the internal carotid plexus
🔸Inferior or Stellate ganglion is fused with the first thoracic ganglia
THORACIC SYMPATHETIC GANGLIA
🔸T1-T5 ganglia supply the aortic, cardiac and pulmonary plexus
🔸The last 7 thoracic ganglia form the greater and lesser splanchnic nerves
🔸The lowest splanchnic nerve is formed from the last thoracic ganglia and supplies the renal plexus
LUMBAR PREVERTEBRAL SYMPATHETIC GANGLIA
🔸Supplies the coeliac plexus
SACRAL SYMPATHETIC GANGLIA (PELVIC)
🔸Contribute to hypogastric and pelvic plexus
➿The autonomic nervous system is a division of the nervous system that controls the activity of internal organs.
➿The sympathetic division prepares the body for fight or flight reactions. The parasympathetic system promotes ‘rest and digest’ (restorative) functions.
➿Acetylcholine is the principal transmitter released by the preganglionic fibres of both the sympathetic and the parasympathetic nervous systems. The parasympathetic postganglionic fibres secrete acetylcholine onto their target organs, whereas norepinephrine is principally secreted by the postganglionic sympathetic fibres.
➿The central portions of the autonomic nervous system are located in the hypothalamus, brainstem and spinal cord. The limbic system and parts of the cerebral cortex send signals to the hypothalamus and lower brain centres, which can also influence the activity of the ANS
➿The posterior and lateral hypothalamic areas increase blood pressure and heart rate, whereas the preoptic area decreases blood pressure and heart rate. These effects are mediated by cardiovascular centres in the pontine and medullary reticular formation.
➿In the ANS, the connection between the CNS and its effector consists of two neurons—the preganglionic neuron and the postganglionic neuron. The synapse between these two neurons lies outside the CNS, in an autonomic ganglion [These are the cell bodies of the post ganglionic neuron, located in chains alongside the vertebral column, in plexuses in the abdomen (Sympathetic) or within the innervated target organ (Parasympathetic)]. The axon of a preganglionic neuron enters the ganglion and forms a synapse with the dendrites of the postganglionic neuron. The axon of the postganglionic neuron emerges from the ganglion and travels to the target organ #TheLayMedicalMan
➿The sympathetic system has short preganglionic fibres and long postganglionic fibres. As the parasympathetic ganglia are located near or within their effector organs, the parasympathetic postganglionic fibres are short.
➿ The pre-ganglionic fibres are slow-conducting B or C fibres. The postganglionic fibres that originate from the ganglia and innervate target organs are largely slow-conducting, unmyelinated C fibres. #TheLayMedicalMan
➿ There are more postganglionic fibres than preganglionic nerves and so the stimulation of a single preganglionic neuron can activate many postganglionic nerves, resulting in divergence. But in the superior cervical ganglion, numerous preganglionic fibres converge on a single postganglionic neuron, resulting in convergence.
Facebook page : Anesthesia Info from The Lay Medical Man
🎳The anterior hypothalamus controls the parasympathetic nervous system
🎳The posterior and lateral hypothalamic areas increase blood pressure and heart rate, whereas the preoptic area decreases blood pressure and heart rate.
🎳The parasympathetic nervous system arises from neurons in the brainstem and spinal cord sacral segments (S 2 –S 4 ). As the parasympathetic ganglia are located near or within their effector organs, the parasympathetic postganglionic fibres are short, and they all release acetylcholine. The distribution of parasympathetic outflow is restricted so that parasympathetic effects are more localized than sympathetic effects.
🎳Cranial nerves 3, 7, 9 and 10 have parasympathetic components (3 – pupil and ciliary body constriction; 7 – tearing and salivation; 9 -salivation: 10 – the vagus and its ramifications).. Preganglionic fibres of the third cranial nerve arise from the oculomotor nucleus and pass through the orbit to the ciliary ganglion. Postganglionic fibres from the ciliary ganglion supply the ciliary muscle and sphincter of the iris and constrict the pupils.
🎳Preganglionic fibres from the superior salivary nucleus of the seventh nerve form the chorda tympani and reach the submaxillary ganglion via the lingual nerve. Postganglionic fibres supply the submaxillary and sublingual salivary glands and cause salivary secretion. #TheLayMedicalMan
🎳Preganglionic fibres arising from the inferior salivary nucleus of the ninth nerve form the lesser superficial petrosal nerve and reach the otic ganglion. The postganglionic fibres are distributed to the parotid gland via the auriculotemporal nerve and also cause salivary secretion.
🎳The vagus nerve is the major part of the cranial parasympathetic outflow. The preganglionic fibres arise from the dorsal nucleus of the vagus in the medulla and terminate in the ganglia of plexuses or in the walls of visceral organs. Postganglionic fibres supply the heart and decrease cardiac excitability, contractility, conductivity and rate. Postganglionic fibres from the pulmonary plexus contract the circular muscles of the bronchi, producing bronchoconstriction. Vagal branches to the gastric plexus give rise to postganglionic fibres to the stomach, liver, pancreas and spleen. Stimulation of the vagus causes increased gastric motility and secretions, with relaxation of the pyloric sphincter. The intestinal branches of the vagus supply the small and large intestines down to the transverse colon and it’s stimulation increases peristalsis and relaxes the ileocolic sphincter. #TheLayMedicalMan
🎳 The sacral outflow of the parasympathetic system arises from the second, third and fourth sacral segments of the spinal cord, and fibres enter the hypogastric plexus to innervate the descending colon, rectum, bladder and uterus. It’s stimulation contracts the muscular wall of the rectum, relaxes the internal sphincter of the anus and contracts the detrusor muscle of the bladder wall.
Ref: Principles of Physiology for the Anaesthetist , 3/e
#physiology , #anaesthesia
🔸Posterior hypothalamus is the principal site of sympathetic nervous outflow.
🔸The sympathetic system has short preganglionic fibres and long postganglionic fibres
🔸The sympathetic nerves originate from columns of preganglionic neurons in the grey matter of the lateral horn of the spinal cord from the first thoracic segment down to the second or third lumbar segment.
🔸’BASIC CIRCUIT’ : PREGANGLIONIC NEURONS in the grey matter of the lateral horn of the spinal cord (from T1-L3 segment) –> they leave the spinal cord through the VENTRAL roots with the spinal nerves and then leave the spinal nerves as WHITE RAMI COMMUNICANTES (myelinated B fibres)–> they then synapse with the POSTGANGLIONIC NEURONS in the GANGLIA OF THE SYMPATHETIC CHAIN –> These ganglia together will form sympathetic chains –> The POSTGANGLIONIC NEURONS leave the ganglia as GREY RAMI COMMUNICANTES (unmyelinated C fibres) and join the spinal nerves or visceral nerves to innervate the target organ.
🔸In general, the preganglionic fibres secrete acetyl choline as neurotransmitter, while the post ganglionic ones secrete norepinephrine. The postganglionic sympathetic nerves that innervate the blood vessels of muscles, sweat glands and the hair follicles in the skin release acetylcholine instead of norepinephrine (noradrenaline).
➡️ The sympathetic chains extend down the length of the vertebral column and are divided into four parts:
🔸A cervical part consisting of superior, middle and inferior galglia, supplying the head, neck and thorax. The superior cervical ganglion sends postganglionic fibres to form the internal carotid plexus. The inferior cervical or stellate ganglion is fused with the first thoracic ganglion.
🔸Branches of the thoracic part, from T1 – T5 supply the aortic, cardiac and pulmonary plexuses. The greater and lesser splanchnic nerves are formed from the lower seven thoracic ganglia. The lowest splanchnic nerve arises from the last thoracic ganglion and supplies the renal plexus.
🔸The coeliac plexus is derived from the lumbar sympathetic ganglia
🔸The sacral ganglia contribute to the hypogastric and pelvic plexus #TheLayMedicalMan
SYMPATHETIC SYSTEM UNIQUE EFFECTS:
DILATATION / RELAXATION
✔️Pupils
✔️Bronchial smooth muscle
✔️Gut, Urinary bladder (sphinctors constrict)
✔️Skeletal muscle arterioles (Post ganglionic transmitter: ACh)
CONSTRICTION / SECRETION
✔️Levator Plapabrae Superioris
✔️Piloerection hair follicle (Post ganglionic transmitter: ACh)
✔️Muscles of seminal vesicles(ejaculation)
✔️Sweat glands (sweating) (Post ganglionic transmitter: ACh)
#physiology , #anaesthesia
Mannitol is a monosaccharide available as 10% & 20% solutions
DURING NEUROSURGERY/ IN NEUROCRITICAL CARE:
✔️Mannitol is freely filtered in the glomerulus but won’t get reabsorbed in the tubules; so it will drive water from the interstitium which gets eliminated as urine. Hence acts as an osmotic diuretic
✔️When blood brain barrier is intact, the osmotic gradient created by mannitol will move water from the cerebral extravascular compartment to the intravascular space, reducing ICP. If blood brain barrier is not intact, it will worsen cerebral edema.
✔️The expansion of the plasma volume caused by mannitol will reduce the viscosity and improve cerebrovascular microcirculation and oxygenation. The increase in cardiac output can also cause an increase in regional blood flow which will cause a compensatory cerebrovascular vasoconstriction in areas where autoregulation is intact.
IN CRUSH INJURY / MYOGLOBINURIA
✔️Will release renal prostaglandins, which will cause renal vasodilation and increase tubular urine flow causing a solute washout and avoidance of tubular obstruction #TheLayMedicalMan
MECHANISM BEHIND ADVERSE EFFECTS
✔️The initial increase in plasma volume as a result of drawing of water into the vascular component and the resultant increase in cardiac output can precipitate heart failure in cardiac patients
✔️The osmotic diuresis can cause hypernatremia [increases urinary losses of both sodium and electrolyte-free water] , metabolic acidosis and hyperosmolarity. It has been advised that therapy should be monitored and titrated so that osmolarity doesn’t go up beyond 300 mOsm/L
✔️The rise in the plasma potassium concentration following hypertonic mannitol is due to the movement of potassium out of the cells into the extracellular fluid as the rise in cell potassium concentration induced by water loss favors passive potassium exit through potassium channels in the cell membrane
✔️Though it has been used for renal protection, the reduction in renal perfusion resulting from hypovolemia caused by diuresis can adversely affect renal function; so should be avoided in patients with renal dysfunction
#Neuroanesthesia , #Anesthesia , #Neurology , #CriticalCare
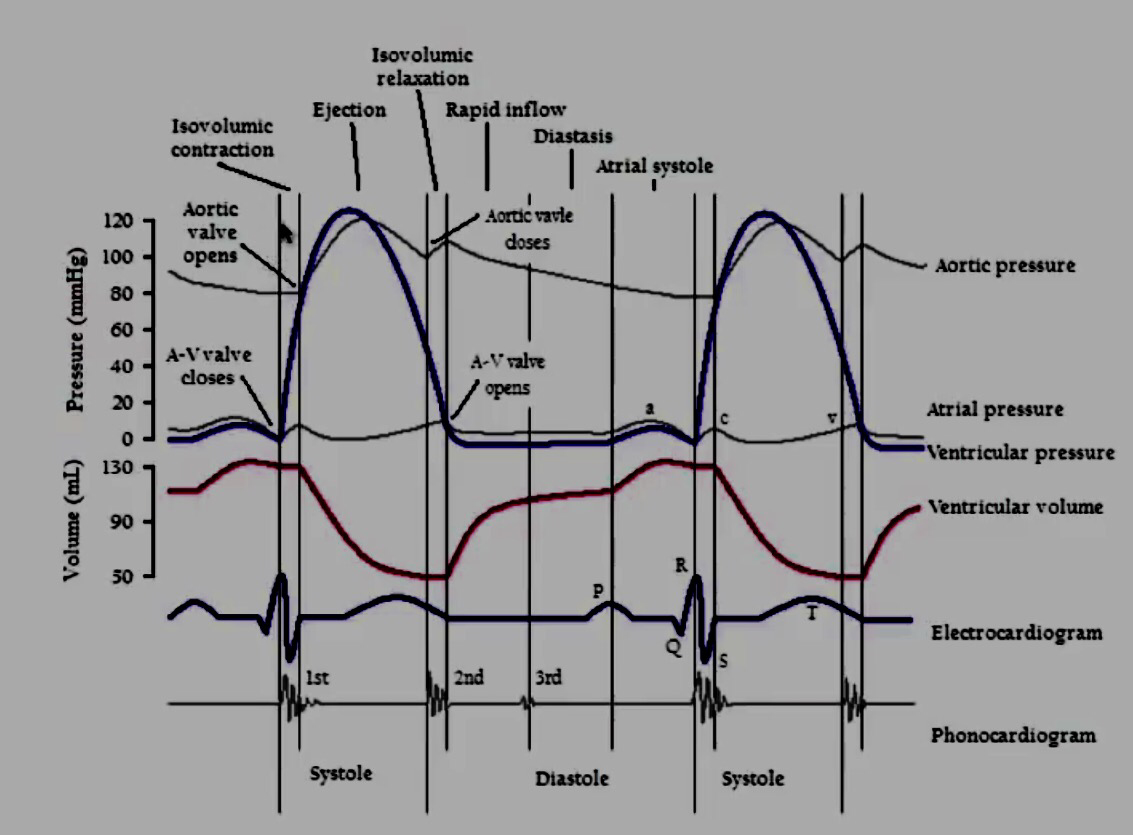
1. ATRIAL CONTRACTION (Phase 1): It is initiated by the P wave of the ECG which represents electrical depolarization of the atria. Atrial contraction does produce a small increase in venous pressure that can be noted as the “a-wave“. Just following the peak of the a-wave is the x-descent. Atrial contraction normally accounts ONLY for about 10% of left ventricular filling when a person is at rest. At high heart rates when there is less time for passive ventricular filling, the atrial contraction may account for up to 40% of ventricular filling. This is sometimes referred to as the “atrial kick.” The atrial contribution to ventricular filling varies inversely with duration of ventricular diastole and directly with atrial contractility. The volume of blood at the end of the filling phase is the end diastolic volume and is around 120 mL in the adult. S4 sound is caused by vibration of the ventricular wall during atrial contraction. Generally, it is noted when the ventricle compliance is reduced (“stiff” ventricle) as occurs in ventricular hypertrophy and in many older individuals.
2. Isovolumetric Contraction (Phase 2): This phase of the cardiac cycle begins with the appearance of the QRS complex of the ECG, which represents ventricular depolarization. The AV valves close when intraventricular pressure exceeds atrial pressure. Closure of the AV valves results in the first heart sound (S1). During the time period between the closure of the AV valves and the opening of the aortic and pulmonic valves, ventricular pressure rises rapidly without a change in ventricular volume (i.e., no ejection occurs). Ventricular volume does not change because all valves are closed during this phase. Contraction, therefore, is said to be isovolumetric. The “c-wave” noted in the venous pressure may be due to bulging of A-V valve leaflets back into the atria. Just after the peak of the c wave is the y’-descent.
3. Rapid Ejection (Phase 3): Ejection begins when the intraventricular pressures exceed the pressures within the aorta (~80 mm of Hg) and pulmonary artery, which causes the aortic and pulmonic valves to open. Left atrial pressure initially decreases as the atrial base is pulled downward, expanding the atrial chamber. Blood continues to flow into the atria from their respective venous inflow tracts and the atrial pressures begin to rise. This rise in pressure continues until the AV valves open at the end of phase 5.
4. Reduced Ejection (Phase 4): Approximately 200 msec after the QRS and the beginning of ventricular contraction, ventricular repolarization occurs as shown by the T-wave of the electrocardiogram. Repolarization leads to a decline in ventricular active tension and pressure generation; therefore, the rate of ejection (ventricular emptying) falls. Ventricular pressure falls slightly below outflow tract pressure; however, outward flow still occurs due to kinetic (or inertial) energy of the blood. Left atrial and right atrial pressures gradually rise due to continued venous return from the lungs and from the systemic circulation, respectively.
5. Isovolumetric Relaxation (Phase 5): When the intraventricular pressures fall sufficiently at the end of phase 4, the aortic and pulmonic valves abruptly close (aortic precedes pulmonic) causing the second heart sound (S2) and the beginning of isovolumetric relaxation. Valve closure is associated with a small backflow of blood into the ventricles and a characteristic notch (incisura or dicrotic notch) in the aortic and pulmonary artery pressure tracings. Although ventricular pressures decrease during this phase, volumes do not change because all valves are closed. The volume of blood that remains in a ventricle is called the end-systolic volume and is ~50 ml in the left ventricle. The difference between the end-diastolic volume and the end-systolic volume is ~70 ml and represents the stroke volume. Left atrial pressure (LAP) continues to rise because of venous return from the lungs. During isovolumetric ventricular relaxation, atrial pressure rises to 5 mmHg in the left atrium and 2 mmHg in the right atrium.
6. Rapid Filling (Phase 6): As the ventricles continue to relax at the end of phase 5, the intraventricular pressures will at some point fall below their respective atrial pressures. When this occurs, the AV valves rapidly open and passive ventricular filling begins. The opening of the mitral valve causes a rapid fall in LAP. The peak of the LAP just before the valve opens is represented by the “v-wave.” This is followed by the y-descent of the LAP. A similar wave and descent are found in the right atrium and in the jugular vein. When a third heart sound (S3) is audible during rapid ventricular filling, it is often pathological and is caused by ventricular dilatation.
7. Reduced Filling (Phase 7): As the ventricles continue to fill with blood and expand, they become less compliant and the intraventricular pressures rise. The increase in intraventricular pressure reduces the pressure gradient across the AV valves so that the rate of filling falls late in diastole. In normal, resting hearts, the ventricle is about 90% filled by the end of this phase. In other words, about 90% of ventricular filling occurs before atrial contraction (phase 1) and therefore is passive.
8. Right Vs Left: The major difference between the right and left side of the cardiac chambers, is that the peak systolic pressures of the right heart are substantially lower than those of the left heart, and this is because pulmonary vascular resistance is lower than systemic vascular resistance. Typical pulmonary systolic and diastolic pressures are 24 and 8 mm Hg, respectively.
9. Jugular Venous Pressure Summary: Right atrial pressure pulsations are transmitted to jugular veins. Thus, atrial contractions produce the first pressure peak called the a wave. Shortly thereafter, the second peak pressure called the c wave follows and this is caused by the bulging of the tricuspid valve into the right atrium. After the c wave, the right atrial pressure decreases (‘x’ descent) because the atrium relaxes and the tricuspid valve descends during ventricular emptying. As the central veins and the right atrium fill behind a closed tricuspid valve, the right atrial pressure rises towards a third peak, the v wave. When the tricuspid valve opens at the end of ventricular systole, right atrial pressure decreases again as blood enters the relaxed right ventricle (‘y’ descent). The right atrial pressure begins to rise shortly as blood returns to the right atrium and the right ventricle together during diastole.
 Ref: Principles of Physiology for the Anaesthetist, Peter Kam, Ian Power, http://www.cvphysiology. com
Ref: Principles of Physiology for the Anaesthetist, Peter Kam, Ian Power, http://www.cvphysiology. com
#CardiacCycle , #Physiology , #Anesthesia