- The commonest structure that can be injured by the laparoscope is the distended stomach. So pass a nasogastric tube and aspirate the stomach contents especially if the induction has involved prolonged bag and mask ventilation.
- Regurgitation of gastric contents can happen
- Pulmonary oedema from fluid infusions and the head-down position
- Insufflation is the most hazardous phase; A demonstrable gas embolism can occur in 1 out of 2000 patients; so watch for high insufflating pressures and low flow. Signs of gas embolism include arrhythmia, hypotension, cyanosis and cardiac arrest. The safest technique is to use CO2 for the pneumoperitoneum rather than N2O, because CO2 is more soluble and if an embolism occurs, it will resolve faster. Watch the indicators on the insufflating machine continuously during inflation. Pressure over 3 kPa or total volume insufflated exceeding 5 litres are hazardous. Caval compression and reduced venous return, with lowered cardiac output, may be a consequence of intra-abdominal pressure exceeding 4 kPa.
- The pressure effect of the insufflating gas will also splint the diaphragm and impede the mechanism of breathing.
- Avoid excessive head down tilt, and always be prepared for laparotomy.
- The end-tidal CO2 will rise during the course of a prolonged procedure and minute volume should be adjusted to compensate.
- Pneumothorax and surgical emphysema have been described, associated with prolonged surgery.
- Shoulder-tip pain, from diaphragmatic irritation, is a common postoperative problem.
DIFFERENCES BETWEEN THE TYPES OF HYPOXIA
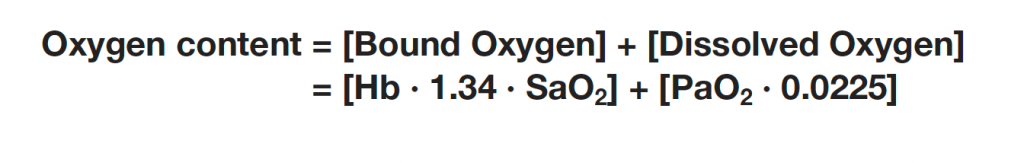
HYPOXIC HYPOXIA (e.g. High Altitude)
- PaO2 is reduced ( as FiO2 is low)
- So more extraction of O2: So PvO2 is reduced
- Based on the above formula, both arterial and venous oxygen content also will be reduced
ANAEMIC HYPOXIA (e.g. haemorhhage)
- PaO2 will be normal
- But arterial oxygen content will be reduced due to lower values of Hb, as per the above formula reducing the oxygen delivery to tissues and increasing the cardiac work
- So there will be more oxygen extraction leading to a low PvO2 and venous oxygen content.
STAGNANT HYPOXIA (e.g. Cardiogenic shock)
- PaO2 is normal
- PvO2 is also normal
- There is no reduction in the arterial and venous oxygen content too.
- However, circulatory dysfunction results in inadequate oxygen delivery to organs
HISTOTOXIC HYPOXIA (e.g. Cyanide poisoning)
- PaO2 is normal. Arterial oxygen content also will be normal.
- But cells are unable to utilise oxygen resulting in high venous saturations
Volume of Distribution
- Is the theoretical volume into which a drug must distributes to produce the measured plasma concentration
- Unit is mL
- It is measured as Vd= Dose / Co, where Co is the initial plasma concentration from a concentration-time graph
- Lipid solubility, plasma protein binding, tissue protein binding, regional blood flow etc determine the Vd
Acidic and Basic drugs
DO YOU KNOW❓
3 drugs with delayed recovery are weak bases: Diazepam, Midazolam & Etomidate (pKa ranging from 3-6)
5 drugs which are potent analgesics are strong bases: Morphine, Fentanyl, Ketamine, Bupivacaine, Lignocaine (7.5-8.5)
4 most commonly used drugs are weak acids: Paracetamol, Propofol, Atropine, Thiopentone (7.5-11)
LASI (lasix) and SALI (salicylic acid) are strong acids (3-4)
At pH < pKa, acidic drugs become less ionised:
HA ⇌ H+ + A–
At pH < pKa, basic drugs become more ionised as they accept protons:
B + H+ ⇌ BH+
Drugs cross membranes in the un-ionised state and so their pKa and the pH of the surrounding environment affect their rate of absorption. Hence, acidic drugs will be more readily absorbed in the highly acidic stomach, whereas basic drugs are better absorbed in the intestine where pH is higher.
Note: You can not find from pKa whether a drug is acidic or basic
CONTEXT SENSITIVE HALF TIME (CSHT)

- Context sensitive half-time is defined as the time for the plasma concentration to fall to half of the value at the time of stopping an infusion.
- The half time will usually alter in the setting of varying durations of drug infusion
- The higher the ratio of distribution clearance to clearance due to elimination, the greater the range for context-sensitive half-time
- The longest possible context-sensitive half-time is seen when the infusion has reached steady state, when there is no transfer between compartments and input rate is the same as elimination rate
- Draw and label the axes; draw the curve for the drug with the shortest CSHT first before plotting the others
- REMIFENTANIL: Here the elimination always dominates distribution and so there is very little variation in CSHT with time and so it is context insensitive. Draw a straight line starting from the origin and becoming near horizontal after the CSHT reaches 5 min. This demonstrates that the half time is not dependent on the length of infusion as clearance by plasma esterases is so rapid. For remifentanil the longest possible CSHT is only 8 minutes
- PROPOFOL: For propofol the clearance due to elimination is similar to that for distribution into the second compartment, so plasma concentration falls rapidly after a propofol infusion mainly due to rapid elimination with a smaller contribution from distribution. Propofol is not context insensitive as its CSHT continues to rise; however it remains short even after prolonged infusions. Starting at the origin, draw a smooth curve rising steadily towards a CSHT of around 40 min after 8 h of infusion. (NB: CSHT of propofol is 20 minutes after 2 hours of infusion, 30 minutes after 6 hours of infusion and 50 minutes after 9 hours of infusion).
- ALFENTANIL: The curve rises from the origin until reaching a CSHT of 50 minutes around 2 h of infusion. Thereafter the curve becomes horizontal. This shows that alfentanil is also context insensitive for infusion durations of 2 h or longer
- THIOPENTONE SODIUM: The curve begins at the origin but rises more steeply than the others so that the CSHT is 50 min after only about 30 minutes of infusion duration. The curve should be drawn like a slightly slurred build-up exponential reaching a CSHT of 150 min after 8 h of infusion. As the CSHT continues to rise, thiopental does not become context insensitive
- FENTANYL: This is the most complex curve and it begins at the origin and is sigmoid in shape. It should cross the alfentanil line at 2 h duration and rise to a CSHT of 250 min after 6 h of infusion. Again, as the CSHT continues to rise, fentanyl does not become context insensitive.
- It is important to realize that the CSHT does not predict the time to patient awakening but simply the time until the plasma concentration of a drug has fallen by half. For example the patient may need the plasma concentration to fall by 75% in order to awaken
- Decrement time: The time taken for the plasma concentration of a drug to fall to the specified percentage of its former value after the cessation of an infusion designed to maintain a steady plasma concentration (time). The CSHT is, therefore, a form of decrement time when the ‘specified percentage’ is 50%.
- When using propofol infusions, the decrement time is commonly quoted as the time taken to reach a plasma level of 1.2 μ g.ml−1 , as this is the level at which wake up is thought likely to occur in the absence of any other sedative agents.
- It must be remembered that after one CSHT, the next period of time required for plasma concentration to halve again is likely to be much longer. This reflects the increasing importance of the slower redistribution and metabolism phases that predominate after re-distribution has taken place. This explains the emphasis on half-time rather than halflife: half-lives are constant whereas half-times are not!
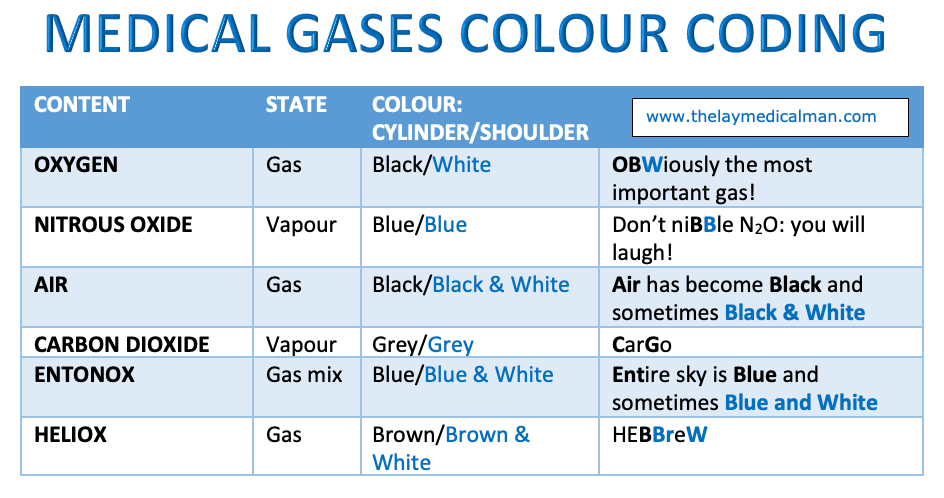
MEDICAL GASES: COLOUR CODING
Antiepileptic of Choice
FOCAL SEIZURE: Lamotrigine, Carbamazepine, Oxcarbamazepine
GENERALISED TONIC CLONIC SEIZURE (GTCS): Sodium Valproate/Lamotrigine/levetiracetam/zonisamide/topiramate
ABSENCE SEIZURE: Ethosuximide/ Sodium Valproate, Lamotrigine (Carbamazepine may exacerbate)
MYOCLONIC SEIZURE: Sodium valproate/ Levetiracetam/ Topiramate/ Zonisamide (Carbamazepine, Lamotrigine may exacerbate)
TONIC/ATONIC SEIZURE: Sodium valproate/Lamotrigine/Phenytoin
INFANTILE SPASMS: Steroids (Prednisolone)/ Vigabatrin
Lennox–Gastaut syndrome: Sodium Valproate/Lamotrigine
(Do not offer sodium valproate to women and girls of childbearing potential)
[Ref: NICE guidelines 2012; last update: 2021 ]
Massive Transfusion and Massive Transfusion Protocol (MTP)
- From a practical standpoint, requirement for > 4 RBC units in 1 hour with ongoing need for transfusion, or blood loss > 150 ml/min with hemodynamic instability and need for transfusion are reasonable definitions in the setting of a massive transfusion situation. Other definitions are >loss of more than one blood volume within 24 hours (around 70 mL/kg, >5 litres in a 70 kg adult), 50% of total blood volume lost in less than 3 hours or bleeding in excess of 150 mL/minute. A pragmatic clinically based definition is bleeding which leads to a systolic blood pressure of less than 90 mm Hg or a heart rate of more than 110 beats per minute.
- Hypoperfusion leads to lactic acidosis, systemic inflammatory response syndrome (SIRS), disseminated intravascular coagulation and multiorgan dysfunction
- Hypoperfusion, acidosis, hemodilution due to iv fluids and progressive hypothermia influences the pathophysiology of massive transfusion in a big way
- Hypothermia and acidosis play a key role by reducing thrombin generation due to altered enzyme kinetics. After 2 weeks of storage, PRBCs have a pH below 7.0, and each unit has an acid load of approximately 6 mEq. Acidosis directly reduces activity of both extrinsic and intrinsic coagulation pathways. A pH decrease from 7.4 to 7.0 reduces the activity of FVIIa and FVIIa/TF by over 90% and 60% respectively. Both coagulation factors and platelets are reduced by hemodilution. NB: High ISS scores, shock, high base deficit and increased INR > 1.5 are associated with increased mortality in the pediatric population
- Collect blood sample for cross match early as colloids may interfere with cross matching (mainly dextrans by coating RBC surface)
- Red cell transfusion is usually necessary if 30–40% blood volume is lost, and rapid loss of >40% is immediately life threatening. Peripheral blood haematocrit and Hb concentration may be misleading early after major acute blood loss. False values occur with TEG too in certain situations. Higher hemoglobin levels reduce TEG/ROTEM signals. Conversely, low hemoglobin makes signals larger.
- ABO-group-specific red cells can usually be issued within 10 minutes of a sample arriving in the laboratory. Fully crossmatched blood is available in 30 to 40 minutes after a sample is received in the laboratory. For immediate transfusion, group O red cells should be issued after samples are taken for blood grouping and crossmatching. Females less than 50 years of age should receive RhD negative red cells to avoid sensitisation.
- Once the volume of blood transfused in any 24 hour period is equivalent to the patient’s own blood volume (8–10 units for adults and 80–100 mL/kg in children), ABO and D compatible blood can be issued without the need for a serological crossmatch.
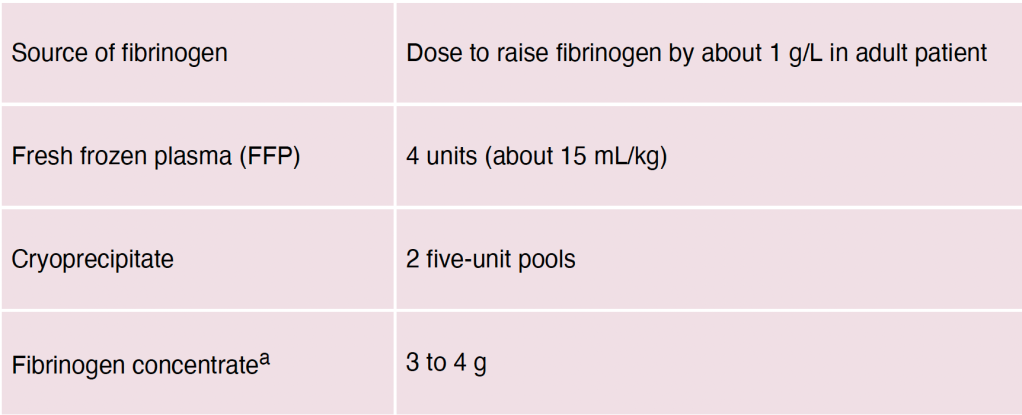
- Fibrinogen Level: Plasma fibrinogen predictably falls to sub-haemostatic levels (<1.5 g/L) after 1 to 1.5 blood volume replacement (earlier in the presence of coagulopathy and hyperfibrinolysis). A threshold level of fibrinogen 1g/L (100 mg/dL) is reached after losing 150% of circulating blood volume as opposed to 200% for clotting enzymes. A fibrinogen level lower than < 1g/L substantially increases in-hospital mortality.
- Coagulation is also impaired by reduced ionised calcium (Ca2+) concentration (which can be measured on many blood gas analysers). Ionised hypocalcaemia may be caused by rapid transfusion of blood components containing citrate anticoagulant, although this is uncommon in the presence of normal liver function
- The fibrinolytic pathway is relatively preserved despite hemodilution. Fibrinolysis is actually increased due to dilution of FXIII and α2 –antiplasmin which reduces fibrin cross-linking, decreases resistance to fibrinolysis and prolongs plasmin half-life. Plasminogen activator inhibitor is decreased, prolonging tissue plasminogen activator (tPA) activity. Stress, thrombin, epinephrine, vasopressin, desmopressin, and bradykinin trigger tPA release. CRASH-2, MATTERs and PED-TRAX studies suggested a survival advantage with administration of Tranexamic Acid.
- FFP should be transfused in doses of 12–15 mL/kg (at least four units in the average adult) to maintain the PT ratio (compared to ‘normal pooled plasma’) less than 1.5. Fibrinogen levels should be maintained above 1.5 g/L
- Large-volume FFP transfusion carries increased risks of circulatory overload (TACO), allergic reactions and transfusion-related acute lung injury (TRALI)
- The platelet count usually remains above 50000/uL (the generally accepted haemostatic level) until 1.5 to 2.5 blood volumes have been replaced. An adult therapeutic dose should be requested when the count falls to 75000-100000/uL.
- Systematic reviews and registry studies show no good evidence of improved survival with the use of recombinant activated factor VIIa and life-threatening arterial and venous thromboembolic complications may occur
- Point‑of‑care testing is highly desirable: Arterial blood gas (ABG) and thromboelastograph (TEG). ABG with haemoglobin (Hb), electrolyte and lactate levels, repeated hourly, are useful in directing therapy
- A few words about citrate toxicity: 80 ml of citrate phosphate dextrose adenine solution present in each blood bag contains approximately 3 g citrate. A healthy adult can metabolise this load in 5 min. However, hypoperfusion or hypothermia associated with massive blood loss can decrease this rate of metabolism leading to citrate toxicity. Unmetabolised citrate can then lead to hypocalcaemia, hypomagnesemia and worsen the acidosis. Hypocalcaemia can lead to myocardial depression that manifests earlier than hypocalcaemic coagulopathy. Hypotension not responding to fluids should alert the physician to this complication. Calcium supplementation is thus required in most cases of massive transfusion
- Massive transfusion protocols (MTP) are generally activated after transfusion of 4-10 units. MTPs have a predefined ratio of RBCs, FFP/cryoprecipitate and platelets units (random donor platelets) in each pack (e.g. 1:1:1 or 2:1:1 ratio) for transfusion. The trigger for initiating the protocol as well as the optimum ratio of RBC: FFP: Platelets is controversial. Therefore practice varies from centre to centre. If MTP is triggered for a nonmassive blood loss situation, it may lead to wastage of blood products.
- Targets of resuscitation in massive blood loss: Mean arterial pressure (MAP) around 60 mmHg, systolic arterial pressure 80-100 mmHg (in hypertensive patients one may need to target higher MAP), Hb 7-9 g/dl, INR <1.5; activated PTT <42 s, Fibrinogen >1.5-2 g/L, Platelets >50000/uL, pH 7.35-7.45, Core temperature >35.0°C, Base deficit <3.0/lactates <2 mEq/L.
The Kappa Test and the Medical Researcher
- Measurement of the extent to which data collectors (raters) assign the same score to the same variable is called interrater reliability (extent of agreement among data collectors)
- Interrater reliability is a concern to one degree or another in most large studies due to the fact that multiple people collecting data may experience and interpret the phenomena of interest differently
- While there have been a variety of methods to measure interrater reliability, traditionally it was measured as percent agreement, calculated as the number of agreement scores divided by the total number of scores; but it will not account for chance agreement. i.e. it does not take account of the possibility that raters guessed on scores. Cohen’s kappa was developed to account for this concern
- Cohen’s kappa, symbolized by the lower case Greek letter, κ is a robust statistic useful for either interrater or intrarater reliability testing.
- Similar to correlation coefficients, it can range from −1 to +1, where 0 represents the amount of agreement that can be expected from random chance, and 1 represents perfect agreement between the raters. While kappa values below 0 are possible, they are unlikely in practice
- Cohen suggested the Kappa result be interpreted as follows: values ≤ 0 as indicating no agreement and 0.01–0.20 as none to slight, 0.21–0.40 as fair, 0.41– 0.60 as moderate, 0.61–0.80 as substantial, and 0.81–1.00 as almost perfect agreement. But there are many arguments against this classification and a modified classification has been recommended
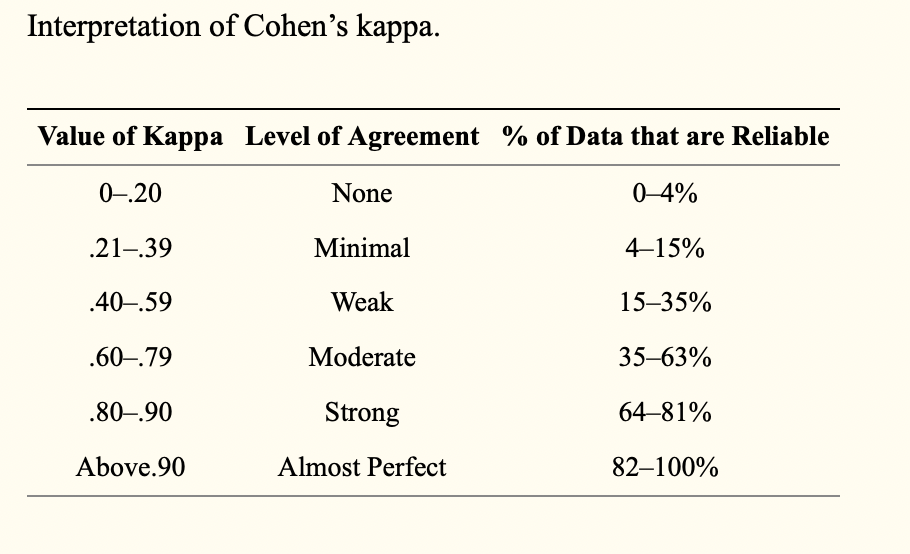
- Any kappa below 0.60 indicates inadequate agreement among the raters and little confidence should be placed in the study
- Kappa may lower the estimate of agreement excessively. Also it cannot be directly interpreted, and thus it has become common for researchers to accept low kappa values in their interrater reliability studies.
- Low levels of interrater reliability are not acceptable in health care or in clinical research, especially when results of studies may change clinical practice in a way that leads to poorer patient outcomes. The best advice for researchers is to calculate both percent agreement and kappa. If there is likely to be much guessing among the raters, it may make sense to use the kappa statistic, but if raters are well trained and little guessing is likely to exist, the researcher may safely rely on percent agreement to determine interrater reliability.
PHENTOLAMINE
- Competitive alpha blocker
- Used in hypertensive emergencies like in pheochromocytoma; also in CRPS
- MOA: 3 times more specific for alpha 1 receptors than alpha 2. Doesn’t bind covalently to receptors; hence reversible. Also has beta agonistic and anti-serotoninergic activity
- Comes as pale yellow solution 10 mg/mL; dose is 1–5 mg titrated to effect
- CVS: Vasodilation and reduce BP, improve coronary artery perfusion, reduce pulmonary artery pressures. Alpha 2 blockade enhances noradrenaline release causing increase in HR and CO
- RESPIRATORY SYSTEM: Increase FEV1, increase secretions, prevents bronchospasm caused by histamine release
- Other Side Effects: Nasal congestion, Hypoglycemia (Causes insulin secretion)
