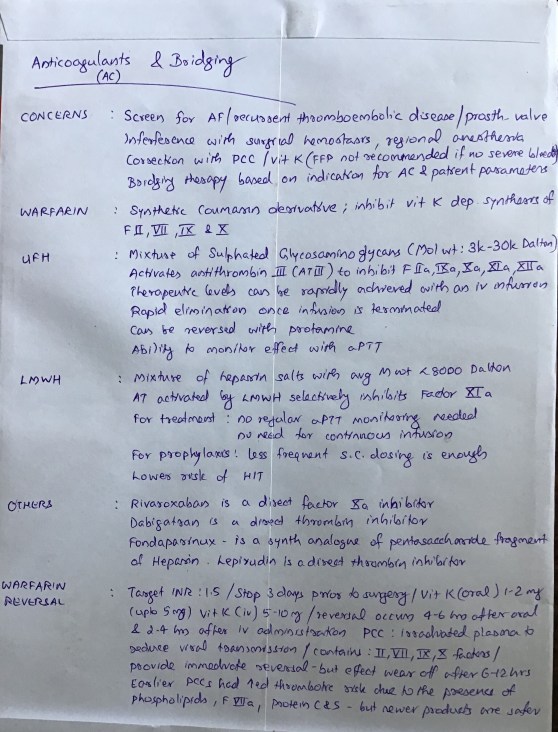
N.B. Corrections:
LMWH inhibits factor Xa (Not XIa)

N.B. Corrections:
LMWH inhibits factor Xa (Not XIa)
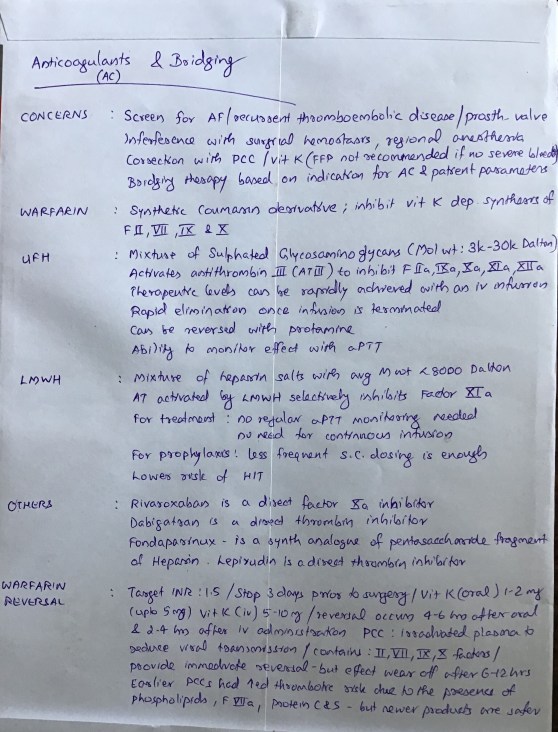
It suppresses adrenocortical function by inhibition of the enzymes 11-hydroxylase and 17-hydroxylase, resulting in inhibition of cortisol and aldosterone synthesis.
induction dose of etomidate represents a massive overdose with respect to its ability to suppress adrenocortical function. And etomidate’ s terminal elimination half-life is rather long. Thus, after just a single anesthetic induction dose of etomidate, many hours must pass before etomidate’ s concentration in the blood falls below that which suppresses adrenocortical steroid synthesis.
It is within this mechanistic context that the strategy emerged to design analogues of etomidate
is very low which means that extremely large doses would need to be administered to maintain anesthesia ]
Involuntary movements (myoclonus) are commonly observed after etomidate administration, with some studies reporting an incidence as high as 80 % in unpremedicated patients
Regardless of the mechanism, myoclonus can be significantly reduced or completely prevented by administering a variety of drugs with central nervous system depressant effects including opiates, benzodiazepines, dexmedetomidine, thiopental, lidocaine, and magnesium.
Pain at the injection site is another common side effect and its incidence is highly dependent upon the size of the vein into which it is injected and the formulation that is used.
Lipid emulsion and cyclodextrin formulations may reduce TRP channel activation, leading to less pain on injection
Postoperative nausea and vomiting is common with reported incidences as high as 40 %. It has been suggested that the emetogenic trigger in etomidate is the propylene glycol solvent and not the anesthetic itself.
Reference: Ref: Pharmacology for Anaesthesia and Intensive Care, Peck and Hill, 4/e, p:105, Total Intravenous Anesthesia and Target Controlled Infusions, A comprehensive global anthology, Anthony R Absalom
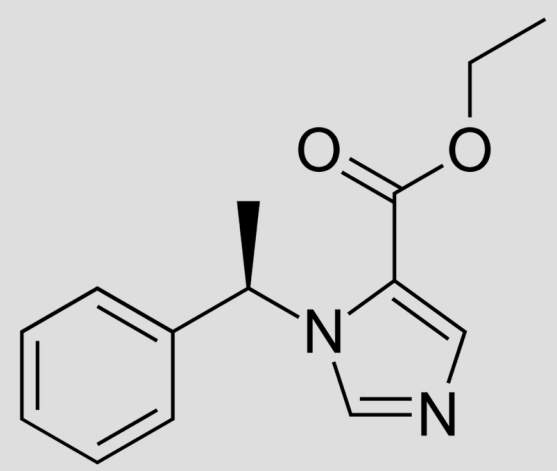
Context sensitive half-time is deined as the time for the plasma concentration to fall to half of the value at the time of stopping an infusion
The half time will usually alter in the setting of varying durations of drug infusion
longest possible CSHT is only 8 minutes
at around 2 h of infusion. Thereafter the curve becomes horizontal. This shows that alfentanil is also context insensitive for infusion durations of 2 h or longer
curve should be drawn like a slightly slurred build-up exponential reaching a CSHT of 150 min after 8 h of infusion. As the CSHT continues to rise, thiopental does not become context insensitive
FENTANYL: The most complex curve begins at the origin and is sigmoid in shape. It should cross the alfentanil line at 2 h duration and rise to a CSHT of 250 min after 6 h of infusion. Again, as the CSHT continues to rise, fentanyl does not become context insensitive.
The maximum possible CSHT for propofol is about 20 minutes, compared with 300 minutes for fentanyl
It is important to realize that the CSHT does not predict the time to patient awakening but simply the time until the plasma concentration of a drug has fallen by half. The patient may need the plasma concentration to fall by 75% in order to awaken, and the time taken for this or any other percentage fall to occur is known as a decrement time.
Decrement time: The time taken for the plasma concentration of a drug to fall to the specified percentage of its former value after the cessation of an infusion designed to maintain a steady plasma concentration (time). The CSHT is, therefore, a form of decrement time when the ‘ specified percentage’ is 50%.
Although the CSHT for propofol has a maximum value of about 20 minutes, during long, stimulating surgery infusion rates will have been high and the plasma concentration when wake-up is required may be very much less than half the plasma concentration at the end of the infusion. Thus time to awakening using propofol alone may be much longer than the CSHT. This is why the TCI pumps display a decrement time rather than a CSHT.
When using propofol infusions, the decrement time is commonly quoted as the time taken to reach a plasma level of 1.2 μ g.ml−1 , as this is the level at which wake up is thought likely to occur in the absence of any other sedative agents.
It must be remembered that after one CSHT, the next period of time required for plasma concentration to halve again is likely to be much longer. This relects the increasing importance of the slower redistribution and metabolism phases that predominate after re-distribution has taken place. This explains the emphasis on half-time rather than halflife: half-lives are constant whereas half-times are not!
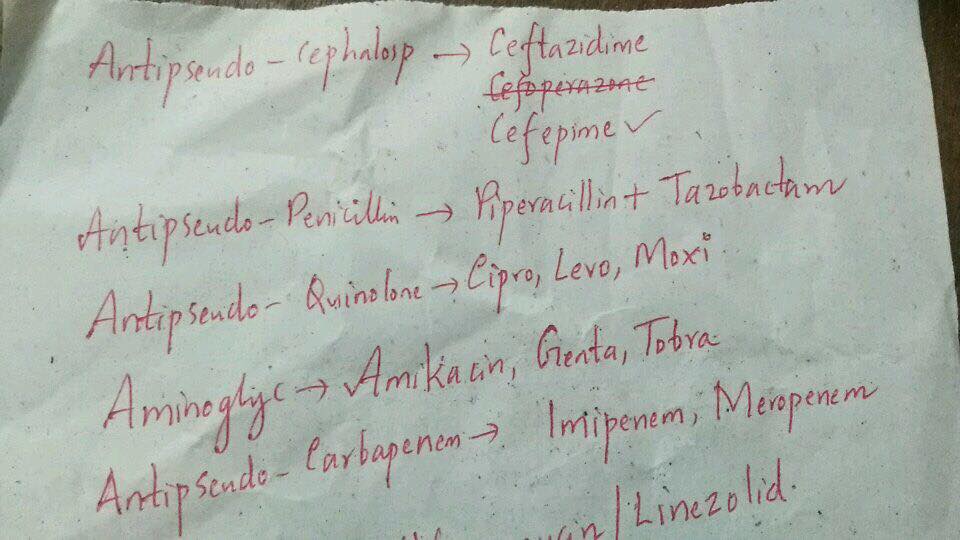
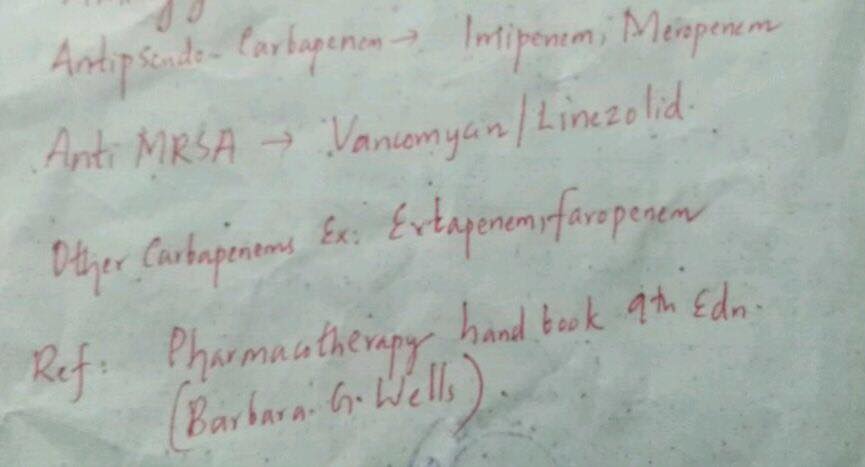
A 70 year-old female is intubated 5 days after hospital admission for hypoxemic respiratory failure after a witnessed aspiration event. Prior to admission, the patient lived in a nursing home, and recently was treated for left leg cellulitis with a short course of intravenous antibiotics. Her medications include metoprolol, metformin, glyburide, atorvastatin, and baby aspirin. Three days after intubation, the patient is noted to have a temperature of 102.5 °F, a blood pressure of 70/50 mmHg, a white blood cell count of 20.0 × 109/L, with purulent secretions suctioned from the endotracheal tube. You decide to initiate antibiotic therapy. Which of the following is the best antibiotic regimen to initiate at this time?
A. Ceftriaxone and ertapenem
B. Imipenem, levofloxacin and vancomycin
C. Meropenem, cefepime, and piperacillin-tazobactam
D. Cefepime and daptomycin
E. Ceftriaxone and azithromycin
Answer: Yes its B!
Healthcare associated infections are almost routine in today’s critical care units, and the increasing rates of multi-drug resistant (MDR) organisms is taking a toll on our clinical and economic systems. Ventilator associated pneumonia (VAP) is a subtype of healthcare associated infection, and is defined by the diagnosis of clinical pneumonia 48–72 h after intubation. Duration of mechanical ventilation, antibiotic use history, geography, co-morbidities, and the epidemiology of the ICU population all determine the etiology of a nosocomial pneumonia. Aerobic gram negative bacilli are the most common pathogens causing VAP. These include Klebsiella, Escherichia coli, Pseudomonas, Acinetobacter, Stenotrophomonas, Enterobacter, Citrobacter, Proteus, and Serratia species. Pseudomonas is the most prevalent pathogen recovered in VAP. With the emergence of MDR organisms, Methicillin resistant Staphylococcus aureus (MRSA) is also an important etiology of VAP, as well as anaerobes such as Bacteroides species. Community acquired pathogens, including Streptococcus and Haemophilus species are less likely to cause VAP. The antibiotic regimen that should be initiated depends on the suspicion that a patient harbors MDR pathogens. Usually, if a patient is hospitalized for more than 5 days, the possibility of MDR pathogens is high, particularly if a patient has been on intravenous antibiotic therapy recently. The first line treatment would include an antipseudomonal cephalosporin or an antipseudomonal carbapenem or an antipseudomonal penicillin with Beta lactamase inhibitor, plus an antipseudomonal fluoroquinolone or aminoglycoside, plus an anti-MRSA agent . Azithromycin should be considered for atypical coverage if Legionella is high on the differential and in severely ill patients. If an MDR pathogen is not suspected, a third-generation cephalosporin or respiratory fluoroquinolone or non-antipseudomonal carbapenem should be considered. Daptomycin is not appropriate to use for pulmonary infections, as it is inactivated by surfactant.
See the pictures for examples of these drug categories
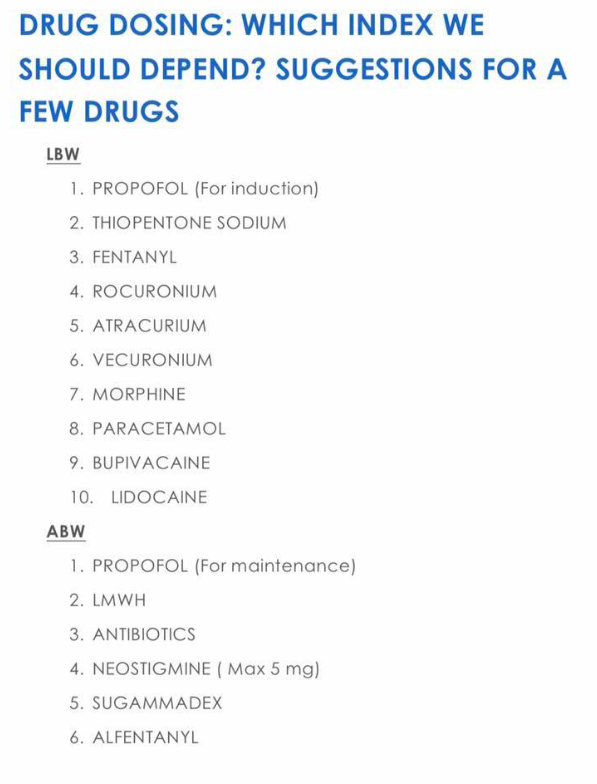
Drug administration in obese patients is difficult because recommended doses are based on pharmacokinetic data obtained from individuals with normal weights
With increasing obesity, fat mass accounts for an increasing amount of TBW, and the LBW/TBW ratio decreases
TBW is defined as the actual weight
IBW is what the patient should weigh with a normal ratio of lean to fat mass
IBW can be estimated from the formula: IBW (kg) = Height(cm) − x ( where x = 100 for adult males and 105 for adult females).
LBW is the patient’s weight , excluding fat
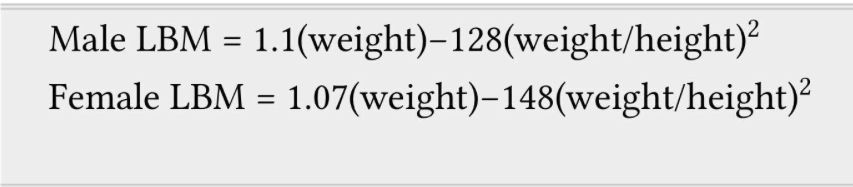
Male LBW = 1.1(weight)-128(weight/height)^2 (Weight in Kg and Height in cm)
Female LBW = 1.07 (weight) -148 (weight/height)^2
Regardless of total body weight, lean body weight rarely exceeds 100 kg in men and 70 kg in women
Below IBW, TBW and LBW are similar.
Adjusted body weight (ABW) Takes into account the fact that obese individuals have increased lean body mass and an increased volume of distribution for drugs.
It is calculated by adding 40% of the excess weight to the IBW : ABW (kg) = IBW (kg) + 0.4 [TBW (kg)]
Drugs with weak or moderate lipophilicity can be dosed on the basis of IBW or more accurately on LBW. These values are not same in obese; because 20–40% of an obese patient’s increase in TBW can be attributed to an increase in LBW. Adding 20% to the ‘estimated IBW based dose’ of hydrophilic medication is sufficient to include the extra lean mass. Non-depolarizing neuromuscular blocking drugs can be dosed in this manner.
In morbidly obese patients, the induction dose of propofol can be calculated on IBW.
In case of midazolam, prolonged sedation can occur from the larger initial dose needed to achieve adequate serum concentrations. #TheLayMedicalMan
Remifentanil dosing regimens should be based on IBW or LBW and not on TBW.
When using succinylcholine in obese adults or adolescents, dosage should be calculated on TBW
The antagonism time of neostigmine has been shown to be independent of TBW and BMI. Therefore, TBW can be used to calculate the dose.
Ref:Association of Anaesthetists of Great Britain and Ireland. Peri-operative management of the obese surgical patient 2015. Anaesthesia 2015, 70, pages 859–876.
FACTS ABOUT THE SURGERY
There is a master console; surgeon sits here & controls the robotic surgical manipulator, once it has been docked
Robot is bulky and is positioned over the chest and abdomen
Patient is positioned in lithotomy with a steep Trendelenberg tilt
Needs immobility of the patient till the robot is undocked
Table position should not be altered until the surgical instruments are disengaged
Discharge may occur as early as within 24 hours after surgery
ADVANTAGES
Better continence & erectile function
Less pain and hence less analgesic requirements
Less blood loss
Shorter hospital stay
ANESTHESIA CONCERNS
Since immobility is very important, it can be established by continuous infusion of a non depolarizing muscle relaxant
As the procedure may take long time, it’s better to use agents with rapid offset
Because patient is positioned in steep head-down position
Ensure pressure points are protected adequately
Fluids are infused cautiously to reduce chances of cerebral and laryngeal oedema ( N.B.: Rule out cerebral oedema in case of delayed emergence )
As the position of the robot interferes with resuscitation, prior practice-drills and good communication are necessary to manage such a situation effectively
Epidural analgesia, if at all required, are used only postoperatively, as the steep head-down position will increase the risk of high block
Reference: Irvine M, Patil V. Anaesthesia for robot-assisted laparoscopic surgery. Contin Educ Anaesth Crit Care Pain. 2009; 9(4): 125–129.
#ProstateSurgery , #RoboticSurgery , #anaesthesia , #perioperative
Low flow anesthesia allows for economy of volatile anesthetics, makes possible heating and humidification of gases and reduces environmental pollution
Sodalime contains 94% Calcium hydroxide, 5% Sodium hydroxide and also Potassium hydroxide, Silica and dying agent
CO2 + 2NaOH –> Na2CO3 + water + heat
Na2CO3 + Ca(OH)2 –> 2NaOH + CaCO3
..this sequence gets back Sodium hydroxide
1 Kg of Sodalime can absorb >120 L of CO2
Carbon monoxide which is a byproduct of protein metabolism can accumulate in the system, but levels are <4%
If there is intoxication by alcohol or poisoning by Carbon monoxide or severe diabetic ketosis, alcohol or CO or acetone from the expired gases, will recirculate and accumulate inside the system; so low flow anesthesia is contraindicated in such states
Prolonged anesthesia with sevoflurane may generate Compound A inside the system, which can cause acute tubular necrosis in rats at concentrations around 250 ppm, a dose that is nearly 200 times seen in clinical practice. So any proteinuria, glycosuria or enzymuria which does develop in such a context has not been shown to have any clinical significance, even in patients with pre-existing renal disease
Reference: Al-Shaikh B, Stacey S. Essentials of Anaesthetic Equipment, 2nd edn. Edinburgh: Churchill Livingstone, 2002; pp. 74–9 . Nunn G. Low-flow anaesthesia. Contin Educ Anaesth Crit Care Pain 2008; 8: 1–4.
Corneal abrasion is the most common ocular complication after general anesthesia
Ischemic Optic neuropathy (ION) and Central Retinal Artery Occlusion (CRAO) are the commonest causes for postoperative visual loss
ISCHEMIC OPTIC NEUROPATHY (ION)
More common among the two
Most often seen after prolonged surgery in prone position
Venous congestion–> Raised Intra Ocular Pressure (IOP) due to Raised Intra Orbital Pressure –> Intra Orbital ‘Compartment Syndrome’
Hypotension, Diabetes, Vascular disease, Smoking etc also may be important in the etiopathogenesis
Treatment:
Reduce optic nerve edema as it passes through posterior scleral foramen with steroids and mannitol
Optimal oxygen delivery by ensuring normal blood pressure and hematocrit
Clear all obstruction to venous drainage
Chance of visual recovery is less
CENTRAL RETINAL ARTERY OCCLUSION (CRAO)
External pressure on eye and embolism are risk factors
An echocardiogram and carotid ultrasound may help us to find an embolic source
Reference: White E, David DB. Care of the eye during anaesthesia and intensive care. Anaesth Intens Care Med. 2007; 8(9): 383–386.