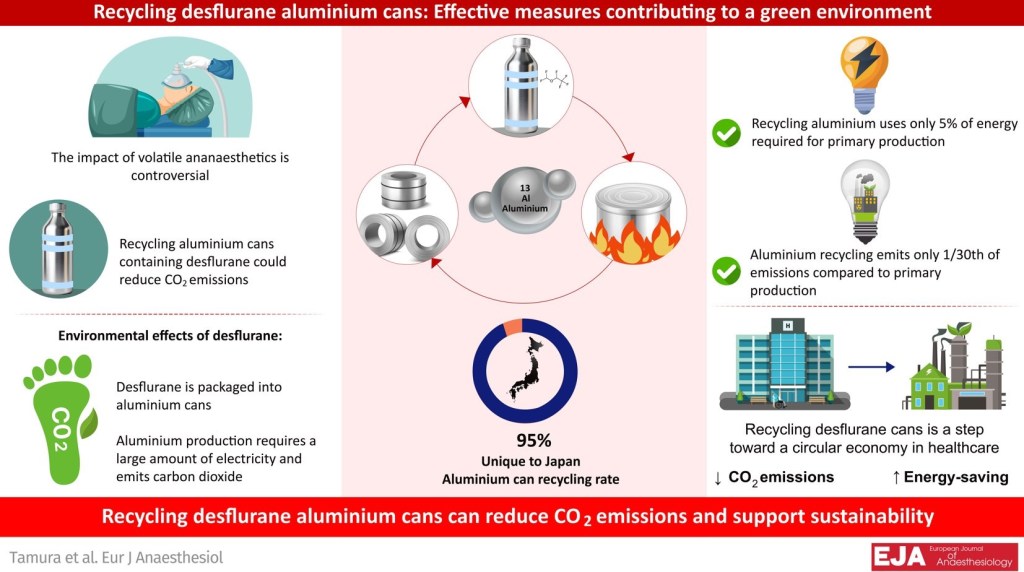
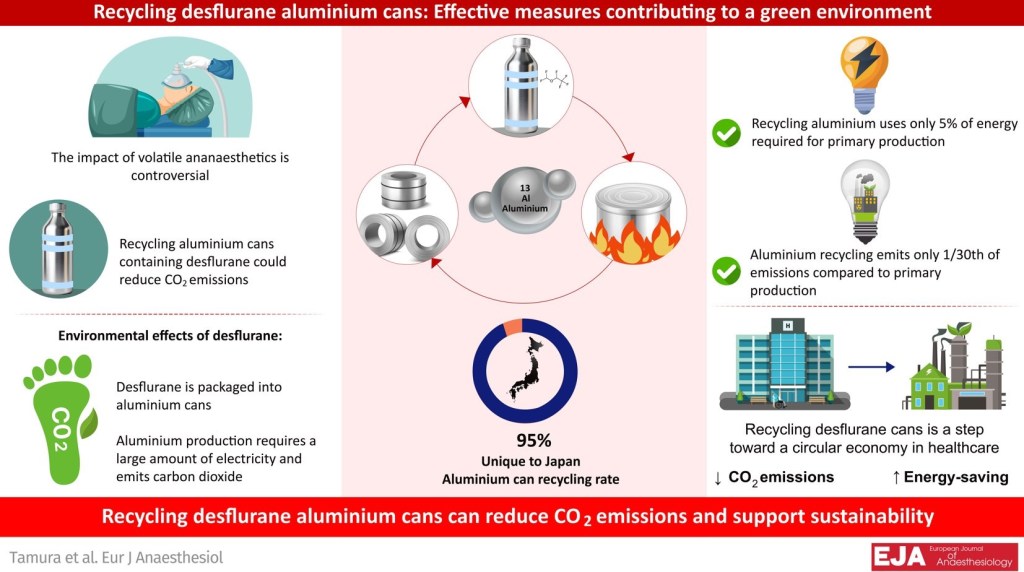
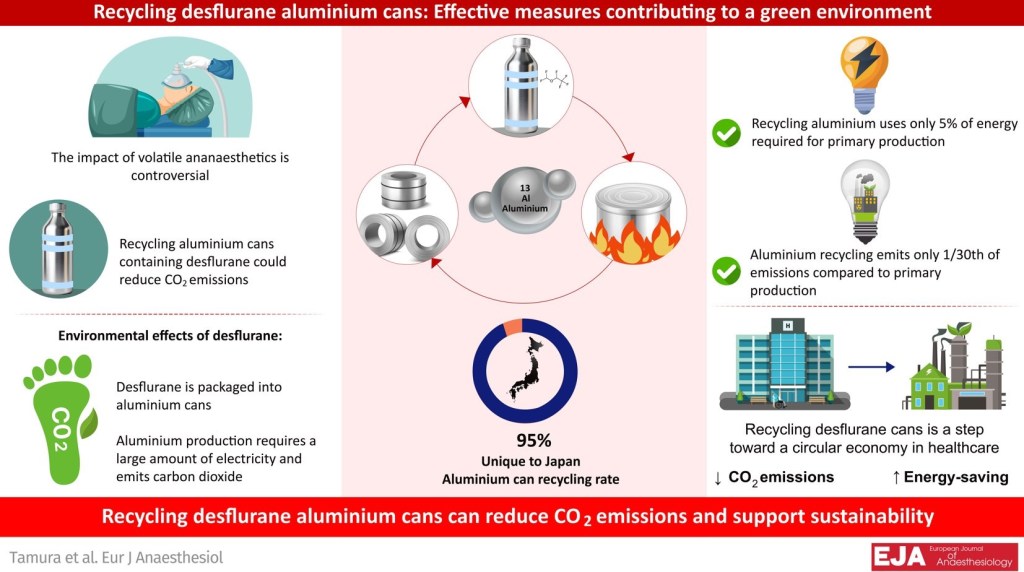
DESFLURANE CANS RECYCLING

Bridging anticoagulation consists of the substitution of a long-acting anticoagulant (usually with warfarin) for a shorter-acting anticoagulant (usually LMWH) to limit the time of subtherapeutic anticoagulation levels and minimize thromboembolic risk. Despite the growing evidence about the limited to nonexistent benefits of bridging therapy, it is still being used on a case-by-case basis. Clinical scenarios that may benefit from bridging therapy are those involving patients with high thromboembolic risk. In several guidelines, the following scenarios have been proposed:
How to bridge?
During the preoperative period:
During the postoperative period:
N.B. : In 2019, a new strategy was published in the PAUSE study, a prospective clinical trial evaluating a standardized approach for perioperative management of DOACs. The interruption scheme used in this study was simple. For high bleeding risk procedures, rivaroxaban, apixaban, and dabigatran were suspended 48 hours before surgery in patients with CrCl>50 ml/min. If the renal function was compromised (CrCl< 50 ml/min), these drugs were interrupted for four days before surgery. For low bleeding risk procedures, rivaroxaban, apixaban, and dabigatran were interrupted 24 hours before surgery in patients with CrCl>50 ml/min. If the renal function was compromised (CrCl <50 ml/min), drugs were suspended two days before the procedure. Regardless of renal function, all drugs were reinitiated at 48 hours for high bleeding risk surgical procedures and 24 hours for low bleeding risk procedures. The 30-day postoperative rate of major bleeding was 1.35% (95% CI, 0%-2.00%) and rate of arterial thromboembolism of 0.16% (95% CI, 0%-0.48%). However, more studies are needed in patients with high surgical bleeding risk, before implementing this in regular clinical practice
Reference:
Perioperative Anticoagulation Management – StatPearls – NCBI by Polania Gutierrez JJ, Rocuts KR. · 2021
https://www.ncbi.nlm.nih.gov/books/NBK557590/

