Various stress-related cardiomyopathy syndromes are
(1) classic Takotsubo cardiomyopathy, which presents as an acute coronary syndrome
(2) left ventricular dysfunction associated with acute intracranial disease, especially Aneurysmal SAH
(3) transient cardiomyopathy, which occurs during other critical illness, especially sepsis, and
(4) transient cardiomyopathy associated with pheochromocytoma and exogenous catecholamine administration
Takotsubo Cardiomyopathy is also known as takotsubo syndrome, broken heart syndrome, ampulla cardiomyopathy, transient left ventricular apical ballooing, apical ballooning syndrome, transient left ventricular dysfunction syndrome, and stress [induced] cardiomyopathy
It was first described in Japan in 1990
Patients don’t have significant epicardial coronary artery disease
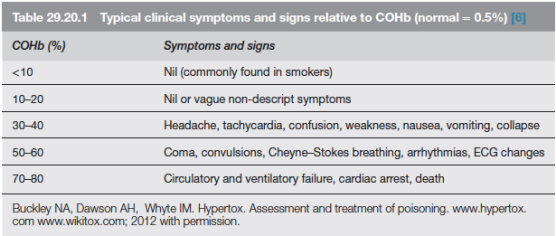
It presents like an acute coronary syndrome ; but symptoms like chest pain, dyspnea, and ECG changes may not be there in all cases
Was most frequently described in postmenopausal elderly women
Was often triggered by stressful situations.
Classic pattern of wall motion abnormality observed is “apical ballooning” usually associated with hyperkinesia of the basal segments ( but its NOT pathognomonic of the disease)
Onset is often preceded / precipitated by emotional or physiologic stress (NOT invariably)
Researchers at the Mayo Clinic proposed diagnostic criteria in 2004, which have been modified recently :
(1) transient hypokinesis, akinesis or dyskinesis in the left ventricular mid segments with or without apical involvement; regional wall motion abnormalities that extend beyond a single epicardial vascular distribution; and frequently, but not always, a stressful trigger
(2) the absence of obstructive coronary disease or angiographic evidence of acute plaque rupture
(3) new ECG abnormalities (ST-segment elevation and / or T-wave inversion) or modest elevation in cardiac troponin; and
(4) the absence of pheochromocytoma and myocarditis.
The most commonly accepted cause is excessive adrenergic/ catecholamine stimulation, which damages cardiomyocytes
Reports of its acute precipitation by administration of catecholamines (like adrenaline or dobutamine) and its reproduction by infusion of adrenaline in primates support this hypothesis
Most patients recover without complications; but others may develop complications like congestive heart failure, pulmonary edema often requiring endotracheal intubation and mechanical ventilation, cardiogenic shock requiring vasopressor or inotropic therapy and even intraaortic balloon pumping
Regarding treatment in the acute phase, avoidance of adrenergic agonists and initiation of antiadrenergic therapy (e.g., adrenergic blocking drugs or centrally acting 2 agonists) have been advocated
In patients presenting with left ventricular outflow tract obstruction, catecholamines are particularly contraindicated
If inotropic therapy is needed (as in case of heart failure, pulmonary edema, and cardiogenic shock etc) there has been suggestions, that the calcium sensitizer levosimendan may be the better choice
One school of thought is that a substantial portion of the damage caused by catecholamine toxicity to the myocardium has likely occurred by the time of clinical presentation, and thus administration of antiadrenergic therapy at this time is unlikely to completely reverse injury. Infact, in a number of reported cases, catecholamines seem to have facilitated recovery in patients with acute left ventricular dysfunction
Reference: anesthesia-analgesia March 2010 • Volume 110 • Number 3 ,circ.ahajournals